Medical | Reflux |
About
|
Coping |
Medication
About Reflux
This section discusses the following about Acid Reflux, GER (Gastroesophageal Reflux), or GERD (Gastroesophageal Reflux Disease) otherwise known as reflux primarily pertaining to infants:
What Is Reflux?
According to Children’s Digestive Health and Nutrition Foundation, (CDHNF) “Gastroesophageal Reflux occurs when an infant’s muscular sphincter-- where the esophagus enters the stomach-- allows acidic, gastric (stomach) fluids to reflux, or flow backwards up into the esophagus and sometimes reach as high as the mouth or nose” (CDHNF, "Coping"). All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
The following are some facts about reflux and GERD:
- "The majority of infants do not experience problems from reflux"1
- "More than 50% of babies spit up regularly in the first months of life"1
- "Reflux usually peaks at 4 months and stops by 12 – 18 months"1
- "Spitting up crosses the line into GERD when the infant begins to show symptoms including refusal to feed, poor weight gain, breathing problems and others."1
- "[R]eflux (GER) and cow milk allergy (CMA) occur frequently in infants younger than 1 year....up to half of cases of GER in infants...may be an association with CMA....[and] also CMA induced."3
- Reflux is "[o]ne of the most common hidden medical causes of nightwaking (and colicky behavior)...."4
- "In many cases GERD in kids can be managed with lifestyle changes, and without medication"1
- "GERD often runs in families"1
- "Kids with GERD may have frequent complaints of abdominal pain or a tummy ache"1
- "Children and teens with asthma are more likely to have GERD"2
1CDHNF, "Quick Facts about Reflux and GERD"
2CDHNF, "Pediatric"
3Salvatore
4Sears, "31 Ways"
Early on I thought my son was suffering from reflux although he was a very happy baby, slept great, and was gaining weight well so we didn't pursue the spitting up issue until my son was around 4 months old and then he no longer wanted to breastfeed or drink his bottle. Then at 6 months he happily ate his baby food for a couple weeks and then would clamp his mouth shut and turn his head away. Once we switched doctors (when my son was around 6 months) he was diagnosed with reflux. The doctor did not order any of the tests to confirm he had reflux since she felt strongly based on the symptoms we described that he suffered from reflux. Please refer to the section below which discusses diagnosing GERD. Please refer to the "Feeding Tricks" article for tips on what we discovered to help our baby eat better when he was suffering from reflux.
(To Top)
Symptoms
Refer below for a list which compiles the symptoms of GERD. I obtained the description of symptoms primarily from the CDHNF web site.
- Crying – "arching away from breast/bottle with crying or irritability"1,2
- Frequent spitting up (although not all babies with GER spit up regularly)2,3
- "Feeding difficulties1,2
- Feeding refusal1,2
- Poor growth or failure to thrive1
- Difficulty eating (e.g., choking or gagging with feeds)"1,2
- "[P]ainful bursts of nighttime fussiness"2,3
- "[F]requent bouts of colicky, abdominal pain"2,3
- "Breathing problems"1
- "Repeat bouts of pneumonia"1
- "Breathing stops"1
- "Turning blue"1
- "Chronic coughing"1,2
- "Wheezing"1,3
- "[T]hroaty sounds" after feeding3
- "Vomiting associated with"1
- "Blood (e.g., bright red streaks, blood clots or coffee ground appearance in stomach fluids)"1
- "Green or yellow fluid"1
- "Poor weight gain"1
- Projectile vomiting2,4
- Hiccups2
- Spitting up milk through nose2
1CDHNF, "Parent's"
2My son's symptom. Note: Hiccups and spitting up milk though nose was not found as a symptom in medical research, this was my personal experience with my son. This may not be a true symptom of reflux although when we tried to wean my son from his reflux medication I noticed he started getting hiccups again. For my son, there tends to be a correlation between hiccups and when his acid reflux acts up.
3Sears, "31 Ways"
4My son's original doctor told us to look out for reflux when my son was 4 months old by watching for projectile vomiting. At 4 months although my son was refusing to eat he was not projectile vomiting. Not all babies with reflux projectile vomit and as discussed by Sears ("31 Ways") some may not even spit up a lot.
Some of my son's symptoms like constant spit-up, spitting up milk through his nose, and hiccups were evident from when he was 1 month old while others like arching away from breast/bottle, feeding refusal, and gagging with feeds occurred when he was 4 months old. My son didn’t projectile vomit until he was older, around six months or so and he didn’t do that very frequently. My son coughed a lot, not a congested cold cough but a cough like he had something stuck in his throat. We use to think he was trying to get attention, little did we know it was due to the reflux.
My son was initially an excellent eater (with his bottle, breastfeeding was not as simple) until around four months and then he had very poor feeding when it came time to drink his bottle or breastfeed. He would cry when we tried to bring the bottle near his mouth. Or if he was drinking he would stop after about an ounce and get very irritable and start arching his back. He also would appear to gag or choke when drinking his bottle. The eating problems continued when at six months for two weeks he happily ate baby food and then he wouldn’t let us even bring the spoon close to his mouth. After switching pediatric doctors we were able to have my son officially diagnosed with reflux at six months and we subsequently started him on reflux medication.
Before the official diagnosis, I was able to help my son drink his bottle and breastfeed by using the "Feeding Tricks" described in that article. I also developed a "Top 10" on introducing baby food to help my son enjoy eating his baby food again. My son was in the 50th percentile for growth and weight for his first year and he stayed in the 50th percentile for growth but dropped back to the 25th percentile for weight in his second year. Once my son was on the medication and we used some of the feeding tips, I felt my son ate well again and by two years old he generally ate extremely well. Our doctor wasn't concerned with his drop in weight during his second year as he said genetics starts to play more of a role and my son's father was very slim as a child.
(To Top)
Diagnosis
Many doctors diagnose the baby based on symptoms described by the parents. Although, if you want to obtain an official diagnosis, the following are some tests performed:
| Type of Test |
Description |
Other Notes |
| Barium Swallow X ray |
This is an X ray test in which the baby drinks "barium which outlines the esophagus, stomach and upper intestines." This test does not diagnose reflux, but helps "exclude other causes...such as anatomical abnormalities of the stomach or intestines that could contribute to or cause a partial obstruction."2 |
When we visited our GI specialist when my son was almost two (and still had reflux) she recommended this test since it is a non-invasive test and would help rule out other problems. She said it would not confirm he had reflux but would let us know if there were any other internal abnormalities. Note: Barium may cause constipation. Our GI specialist said we could give our son MiraLAX after the procedure to help with the constipation. |
| Blood or urine test1 |
|
This seems like a simple procedure but I don't have more information about this test. |
| Endoscopy |
Small camera inserted into baby's esophagus (rarely required to make diagnosis) |
Our GI specialist said she doesn't like to do this test until the baby is older, preferably over three years old as the benefits don't outweigh the risks. Note: The child will need to be put to sleep for the test. |
| pH Monitoring |
The "tube is placed in through your baby's mouth or nose into the esophagus and down to just above the entrance to the stomach." This tests the level of acidity in baby's esophagus.2 |
Our GI specialist doesn't like to do this test until the child is three or older as a younger child won't understand and will try to rip out the tube and it has to be left in for twelve to twenty-four hours. |
| Scintography (Gastric emptying study) |
A computerized scan of baby's abdomen is done to reveal "if the stomach takes a long time to empty (called "delayed gastric emptying")" this does not show "the presence or degree of reflux" but it shows if delayed gastric emptying could be contributing to the reflux.2 |
The baby drinks a radioactive substance in order to do the test. Our GI specialist did not discuss this test. |
| Allergy Test |
Some babies initially diagnosed with reflux actually have a cow milk allergy or another allergy and after switching to a different formula (or having the mom stop drinking milk) the baby is happy. |
You may want to discuss with your doctor the possibility of a milk allergy or another food allergy that may be causing "reflux" symptoms. We temporarily tried using a hypoallergenic formula to see if that helped our baby and it didn't seem to help. |
1CDHNF, "GERD in Infants: Symptoms and Diagnosis"
2Sears, The Baby Book 390 - 391
Our doctor did not run any tests to determine if my son suffered from reflux. She felt very strongly based on our description of his symptoms that he had reflux. It was also evident that once we started him on medication he started eating his baby food again. He still didn't drink his bottle well until almost a year but I do feel the medicine helped with that as well. Later when we tried to wean my son off of the medication he would stop eating and drinking well and would become a more "needy" baby when normally he is extremely independent. For example, he loves going to my gym daycare but the week after I took him off the medication (and sometimes it takes a few days for the medicine to fully wear off) he would cry when I left. Soon as we put him back on his medicine he enjoyed the daycare again. I felt it was like any sick/ hurting child, since he wasn't feeling well he wanted his mommy and once he was well again he could be himself and play and have fun with the other kids.
I continually would ask my son's doctor if we should perform any tests to confirm if he had reflux. He said he doesn't like to do any of the tests unless the child is not growing well or there are other developmental delays. I also asked if I should see a pediatric gastroenterologist (GI specialist), a specialist who cares for children with digestive problems, and my doctor did not think it was necessary. Although, when my son was almost two and didn't seem to be growing out of his reflux and had a bad month of throwing up (primarily due to a cold, he was congested and when he coughed on the mucus he would throw up) I decided it was time to see a GI specialist.
I was extremely happy we went to the appointment. She confirmed again that based on the symptoms described my son seemed to definitely have acid reflux. She increased the medication we were giving him as she said the most important thing is to make sure his esophagus does not get damaged from the acid. In addition, she recommended we do the barium swallow X ray to rule out any other abnormalities that could contribute to the reflux. We did the test and the test was able to confirm that my son's internal system looked "normal" and I was happy to have spent the $200 to learn my son was "healthy" and hope that he will eventually grow out of his reflux.
(To Top)
Treatment
Your pediatrician may recommend a trial of medication that decreases acid in your baby's stomach or refer you to a GI specialist. Our son was put on medication when he was six months old and was on it until about 2 1/2 when he finally seemed to grow out of his reflux. Before my son turned 2 1/2 we tried taking him off the medication several times but he usually would stop eating well and become "needy" when he was usually very independent. When my son was around 2 years old at a visit to the GI specialist she increased his medication as she said the most important thing is to make sure his esophagus is not damaged by the acid. Please refer to the "Medication" article for more information.
If the GERD is extreme then surgery may be recommended. There are also "lifestyle adjustments" that can help a baby:
- "Avoid overfeeding"1
- "Don't feed the baby again after he or she spits up (wait until the next feeding time)"1
- "Check with your doctor to see if you are using appropriately sized bottles or nursing the appropriate amount of time"1
- Our baby drank best with the Dr. Brown's bottles."
- Feed half as much twice as often."2
- Starting at 4 months, our baby would only drink a few ounces at a sitting and so we had to do frequent feedings to help ensure he drank enough for the day.
- "Feeding frequently stimulates more saliva production...[and] [s]alivia contains a healing substance...which helps repair the damaged tissues in the esophagus. It also neutralizes stomach acid and lubricates the irritated lining of the esophagus."2
- If possible, breastfeed your baby
- "[E]asy-in, easy-out" since it empties from the stomach faster and usually produces "softer and easier-to-pass stools"2
- "Breast milk is more intestine friendly than formula."2
- I was able to breastfeed my baby until around 6 months and had I known breast milk would have helped his reflux I would have tried to breastfeed longer. Unfortunately, my son's reflux contributed to weaning from breastfeeding early since around 4 months he didn't want to breastfeed (or bottle feed) and so I started doing more bottles so I could track what he was drinking for the day.
- "If your baby is formula-fed, thicken the formula with a small amount of rice cereal"1
- We switched to oatmeal cereal as it was not as constipating as rice cereal was for our baby.
- Try different formulas, our baby digested Nestle Good Start better than other formulas since it was 100% whey rather than the whey/casein mix of most formulas.
- You may want to try a Hypoallergenic formula to see if your baby has a cow milk allergy.
- Make sure you burp baby well as excess "air aggravates reflux"2
- For awhile, we were hesitant with burping our baby since he got so upset when we burped him but really that was the best thing for him. We found that if we gave him his pacifier when we were burping him that it helped.
- Try other bottles to help minimize air intake or make sure baby is properly latched on for breastfeeding.
- "Keep the baby upright for at least 30 minutes after a feeding."1
- Wear your baby to help keep her upright; I think this helped my baby for the first few months.
- Try to not "jostle or vigorously play with baby after feedings"2 I still try to remind our son's Daddy to try to not play too much right after our son (now almost two years old) eats but that is hard for both him and my son to follow.
- Discuss with your doctor about positioning the baby at night to sleep. It is recommended to put the baby to sleep on her back to help avoid SIDS (Sudden Infant Death Syndrome) but if your baby is suffering from reflux you may want to discuss other sleep positions.
- We elevated our baby's mattress. You can also buy sleep positioners some of which are elevated for the baby. We should have bought one of these.
- "Try not to let your baby spend too much time in a car seat (The baby's position in the car seat can promote reflux)"1
- "Avoid tight diapers and elastic waistbands"1
- Develop parenting style to promote attachment parenting to help decrease crying, "since crying puts pressure on the stomach which worsens the reflux"2
- Pacifier use may help since "sucking stimulates saliva production"2 unless the baby sucks too hard and swallows air then the air can make the reflux worse.
- My son always loved his pacifier and I was happy to let him use something that made him feel better.
- My son is almost two and I still let him have his pacifier for nap and bedtime. I plan to wean in the next year although since he is still suffering from reflux I'm reluctant to wean him. My son's pediatric dentist said we should try to wean him before he turns four. I don't think we should have a problem with that.
- Help baby avoid constipation since "increasing abdominal pressure...can aggravate reflux"2
- Unfortunately, my son had constipation for most of his first year which probably didn't help his reflux.
- Oatmeal cereal was less constipating than rice cereal
- When starting baby food, make sure you avoid or limit the constipating foods like bananas, carrots, and applesauce.
- The "Constipation" article is coming soon
1CDHNF, "GERD in Infants: Treatment and Management"
2Sears, The Baby Book 392 - 397
For other tips on how to help both you and your baby cope with reflux, please refer to the "Coping" article which is coming soon.
(To Top)
End Note
The fact my son had reflux and subsequently developed feeding problems, which we were able to help him eat with "Feeding Tricks" and also "Top 10" with introducing baby food, was a strong contributing factor to why I started this web site. I did a lot of research on reflux and I wanted to share what I learned with others. Although, when it came time to publish this section, it was hard for me to finish writing the reflux articles. I think I had "lived and breathed" so much about reflux that I just didn't want to write any more about it. But I finally decided it was time to publish the articles as I want to share what I learned to help you along your parenting journey. I wish you the best of luck.
Please make sure you discuss any concerns you might have about your baby with your healthcare professional and remember "that with treatment, severe reflux and GERD can improve. A pediatrician or a pediatric gastroenterologist can help your child, and can offer you strategies for coping with GERD. Once your baby's GERD is under control, he or she should enjoy a happy, healthy childhood" (CDHNF, "GERD in Infants: Pediatric").
(To Top)
Works Cited
Children's Digestive Health and Nutrition Foundation (CDHNF). "GERD in Infants: Pediatric GERD in
Infants." 1 April 2010 <http://cdhnf.org/wmspage.cfm?parm1=43>.
---. "GERD in Infants: Symptoms and Diagnosis." 31 March 2010
<http://cdhnf.org/wmspage.cfm?parm1=44>.
---. "GERD in Infants: Treatment and Management." 31 March 2010
<http://cdhnf.org/wmspage.cfm?parm1=36>.
---. "Parent's Checklist for REFLUX in Infants 0-12 months old." 29 March 2010.
<http://cdhnf.org/user-assets/documents/pdf/GERD_Checklist.pdf>.
---. "Pediatric Reflux and GERD." 29 March 2010 <http://cdhnf.org/wmspage.cfm?parm1=42>.
Children's Digestive Health and Nutrition Foundation (CDHNF), et al. "Coping When Your Baby Has
Reflux or GERD: You Are Not Alone." CDHNF. 23 March 2010
<http://cdhnf.org/user-assets/documents/pdf/Coping_Reflux_GERD_Guide.pdf>
Salvatore, Silvia M.D., and Yvan Vandenplas M.D. "Gastroesophageal Reflux and Cow Milk Allergy: Is
There a Link?" Pediatrics: Official Journal of the American Academy of Pediatrics.
110 (2002): 972-984. 30 Oct 2009 <http://pediatrics.aappublications.org>.
Sears, William M.D., Martha Sears, R.N., Robert Sears, M.D. and James Sears, M.D. The Baby Book:
Everything You Need to Know About Your Baby - From Birth to Age Two. New York: Little, 2003.
Sears, William M.D., Martha Sears, R.N., James Sears, M.D., and Robert Sears, M.D. "31 Ways to Get
Your Baby to Go to Sleep and Stay Asleep Easier." AskDrSears.com. 26 Jan 2010
<http://www.askdrsears.com/html/7/T070300.asp>.
(To Top)
Last updated: April 2010
 All Articles
All Articles All Videos
All Videos
 Hot Topics
Hot Topics Breastfeeding &
Breastfeeding &  Home
Home Videos
Videos Blog
Blog Bottle Feeding
Bottle Feeding Bottles
Bottles Formula
Formula Formula Transition
Formula Transition Nipples
Nipples Breastfeeding
Breastfeeding  To or Not To
To or Not To About
About Accessories
Accessories Pumping
Pumping Tips
Tips Comfort Chair
Comfort Chair Feeding Tricks
Feeding Tricks How Much?
How Much? Medical:
Medical: Storing
Storing Cereal
Cereal Water
Water Weaning
Weaning Bottle
Bottle Breast
Breast Nighttime
Nighttime Whole Milk
Whole Milk My Favorite
My Favorite  Resources
Resources Food
Food Home
Home Videos
Videos Blog
Blog Baby Cereal
Baby Cereal Baby Food
Baby Food Baby Food,
Baby Food, How Much to
How Much to Introducing
Introducing Medical:
Medical: Picky Eater
Picky Eater Top 10
Top 10 Water
Water Whole Milk
Whole Milk Organic
Organic Gift of Health
Gift of Health Grocery List
Grocery List Halloween
Halloween Healthy Snacks
Healthy Snacks Meal Ideas
Meal Ideas Dinner
Dinner Resources
Resources My Favorite
My Favorite Resources
Resources Household Items
Household Items Making Memories
Making Memories Home
Home Videos
Videos Blog
Blog Holidays
Holidays Easter Egg
Easter Egg Spring
Spring Summer
Summer Journal
Journal Memory of the Day
Memory of the Day Pictures
Pictures Holiday
Holiday Meal Time
Meal Time Monthly
Monthly Stories
Stories Medical
Medical Home
Home Blog
Blog Colic?
Colic? Reflux
Reflux About
About Coping
Coping Medication
Medication Autism
Autism How to Talk
How to Talk Sick
Sick Cold
Cold Ear Infection
Ear Infection Fever
Fever Middle of
Middle of  Vomiting
Vomiting My Favorite
My Favorite Resources
Resources Parenting
Parenting Home
Home Videos
Videos Blog
Blog Attachment
Attachment Baby Wearing
Baby Wearing About
About Products
Products Cry
Cry Colic?
Colic? Meanings
Meanings Get Easier?
Get Easier? Gift of Health
Gift of Health Nighttime
Nighttime Schedule
Schedule Schedule or Demand
Schedule or Demand Document
Document Template
Template Soothing Techniques
Soothing Techniques Toddlers, Loveable Puppies
Toddlers, Loveable Puppies Obstinate Ones
Obstinate Ones Autism
Autism How to Talk
How to Talk Reading Program
Reading Program Sexual
Sexual Stress Free
Stress Free My Favorite
My Favorite Resources
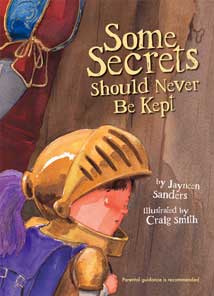
Resources Secrets
Secrets Play Time
Play Time Home
Home Videos
Videos Blog
Blog Costume
Costume  Crafts Ideas
Crafts Ideas Exercise
Exercise Triathlon
Triathlon Infant Play
Infant Play Toddler Play
Toddler Play Preschool Play
Preschool Play Preschool
Preschool  Home
Home Videos
Videos Colors
Colors Reading
Reading My Favorite
My Favorite Resources
Resources Pregnancy &
Pregnancy &  Home
Home Videos
Videos Blog
Blog Pregnancy
Pregnancy Baby Names
Baby Names For Mommy
For Mommy Prepare for
Prepare for  Baby
Baby Delivery
Delivery Take to
Take to Birth
Birth My Favorite
My Favorite Resources
Resources Secrets
Secrets Routine Care
Routine Care Home
Home Blog
Blog Baby Wearing
Baby Wearing About
About Products
Products Car Seat
Car Seat Child Care
Child Care Cry
Cry Colic?
Colic? Help Reduce
Help Reduce Meanings
Meanings Potty Training
Potty Training Reflux
Reflux About
About Coping
Coping Medication
Medication Soothing Techniques
Soothing Techniques Stroller
Stroller Sunblock
Sunblock Autism
Autism How to Talk
How to Talk Sexual
Sexual Stress Free
Stress Free My Favorite
My Favorite Resources
Resources Secrets
Secrets Sleep
Sleep Home
Home Videos
Videos Blog
Blog About
About Amount
Amount Comfort Chair
Comfort Chair Healthy Sleep
Healthy Sleep Nighttime
Nighttime Nightwaking
Nightwaking Behavior
Behavior Medical & Physical
Medical & Physical Parenting
Parenting Routine
Routine Sleep Tips
Sleep Tips Toddler/
Toddler/  You
You Stress Free
Stress Free My Favorite
My Favorite Resources
Resources Travel & Daily
Travel & Daily  Home
Home Blog
Blog Pool Time
Pool Time Holidays
Holidays Easter Egg
Easter Egg Spring
Spring Summer
Summer Vacation
Vacation Busch Gardens
Busch Gardens Busch Gardens Blog
Busch Gardens Blog My Favorite
My Favorite Resources
Resources My Family
My Family Home
Home Videos
Videos Blog
Blog About Me
About Me Journal
Journal Diary of a Mom
Diary of a Mom Diary of a Dad
Diary of a Dad Diary of a 3 Year Old
Diary of a 3 Year Old Diary of an Infant
Diary of an Infant I Love
I Love Let It Snow
Let It Snow Memory of the Day
Memory of the Day New Year's Resolutions
New Year's Resolutions Toddlers, Loveable Puppies
Toddlers, Loveable Puppies Washington Monument
Washington Monument You're a Mom
You're a Mom Meet My Family
Meet My Family Pictures
Pictures Holiday
Holiday Meal Time
Meal Time Monthly
Monthly Stories
Stories Vacation
Vacation Busch Gardens Blog
Busch Gardens Blog My Favorite Things
My Favorite Things Archives
Archives January
January 01/27/2012
01/27/2012 February
February 02/24/2012
02/24/2012 March
March 03/02/2012
03/02/2012 April
April 04/06/2012
04/06/2012 04/27/2012
04/27/2012 May - September
May - September 09/14/2012
09/14/2012 January
January 01/14/2011
01/14/2011 01/21/2011
01/21/2011 01/28/2011
01/28/2011 February
February 02/04/2011
02/04/2011 02/18/2011
02/18/2011 March
March 03/04/2011
03/04/2011 03/25/2011
03/25/2011 April
April 04/21/2011
04/21/2011 May
May 05/06/2011
05/06/2011 05/27/2011
05/27/2011 June
June 06/03/2011
06/03/2011 06/17/2011
06/17/2011 July
July 07/01/2011
07/01/2011 August
August 08/05/2011
08/05/2011 08/25/2011
08/25/2011 September
September 09/09/2011
09/09/2011 09/30/2011
09/30/2011 October
October 10/31/2011
10/31/2011 November
November 11/04/2011
11/04/2011 11/11/2011
11/11/2011 11/18/2011
11/18/2011 December
December 12/02/2011
12/02/2011 12/31/2011
12/31/2011 January
January 01/01/10
01/01/10 01/08/10
01/08/10 01/15/10
01/15/10 01/22/10
01/22/10 01/29/10
01/29/10 February
February 02/05/10
02/05/10 02/12/10
02/12/10 02/19/10
02/19/10 02/26/10
02/26/10 March
March 03/05/10
03/05/10 03/12/10
03/12/10 03/19/10
03/19/10 03/26/10
03/26/10 April
April 04/02/2010
04/02/2010 04/09/2010
04/09/2010 04/16/2010
04/16/2010 04/30/2010
04/30/2010 May
May 05/07/2010
05/07/2010 05/14/2010
05/14/2010 05/21/2010
05/21/2010 05/28/2010
05/28/2010 June
June 06/04/2010
06/04/2010 06/11/2010
06/11/2010 06/18/2010
06/18/2010 06/25/2010
06/25/2010 July
July 07/02/2010
07/02/2010 07/09/2010-
07/09/2010- 07/30/2010
07/30/2010 August
August 08/06/2010
08/06/2010 08/13/2010
08/13/2010 08/20/2010
08/20/2010 08/27/2010
08/27/2010 September
September 09/03/2010-
09/03/2010- 09/17/2010
09/17/2010 October
October 09/24/2010-
09/24/2010- 10/08/2010
10/08/2010 10/15/2010-
10/15/2010- November
November 11/05/2010
11/05/2010 11/12/2010
11/12/2010 11/19/2010
11/19/2010 December
December 12/17/2010
12/17/2010 October
October 10/30/09
10/30/09 November
November 11/13/09
11/13/09 11/20/09
11/20/09 11/27/09
11/27/09 December
December 12/04/09
12/04/09 12/11/09
12/11/09 12/18/09
12/18/09 12/25/09
12/25/09