Please refer to each tab for the respective FAQs.
1. When can I give baby cow's milk?
Please refer to the
"Whole Milk" article.
All research and your doctor generally state that a baby should not drink milk (other than breast milk or formula) if she is less than a year old. “In infants, the introduction of cow’s milk in the first year of life is the greatest dietary risk factor for the development of iron deficiency and iron deficiency anemia.” Not only does cow’s milk not have a lot of iron but the iron in the milk is poorly absorbed. “In addition, it decreases the absorption of iron from dietary sources. Therefore, the strict avoidance of cow’s milk in the first 12 months of life is essential in preventing iron deficiency anemia” (American Academy of Family Physicians (“AAFP”). In addition, the AAFP recommends starting iron supplements at four to six months for breastfed infants and to use iron-fortified formula (NOT low-iron formula) when not breastfeeding.
Another reason not to introduce cow's milk "until at least one year" is because it "is not wise to introduce a potentially allergenic drink at the same time that your baby's intestines are getting used to a variety of solid foods" (Baby 236). You may wonder why some sources recommend giving the baby yogurt or cheese around the nine month mark, doesn't that have milk in it? According to Sears, "[y]ogurt gives all the nutritional benefits of milk but with fewer problems" since the process of making yogurt "breaks down the milk lactose into simple sugars, which are more easily absorbed" and also "making yogurt less allergenic than milk" (Baby, 236). Overall, it is recommended to continue breastfeeding or bottle feeding with formula since formulas are "much closer to the composition of human milk and contain all of the necessary vitamins" until at lest one year (Baby, 236).
(To Top)
2. When can I introduce baby cereal or baby food?
Please refer to the "Baby Cereal," "Baby Food," and "Introducing Baby Food" articles.
Generally, for the first 6 months babies should be entirely breastfed or formula fed. Even once babies start eating solid food, “[t]hey still obtain the vast majority of their calories and nutrition from breast or formula feedings” (Greene, “Introducing”). When the baby is no longer satisfied after drinking a lot of breast milk or formula, usually between 4 to 6 months, a lot of parents start giving the baby cereal.
What are some signs the baby is ready to start solids? According to Dr. Greene,
- Baby still hungry after drinking (8-10 breast feedings or 32 ounces of formula in a day)
- Baby can lift and support her own head
- Baby weighs at least 13 pounds and has doubled her birth weight
- Baby has overcome the strong tongue-thrust reflex they are born with (“When”)
(To Top)
3. How do I introduce baby food?
Please refer to the "Introducing Baby Food" article.
Most research recommends to offer only one new food at a time and wait between 3 days to a week before offering another new food. I generally waited at least a few days when introducing each food as if you do offer multiple foods at once and your baby does have a reaction then you won't know what food caused the reaction.
Top 10 - Get Baby to Eat
10. Make sure baby well rested.
9. Make sure no medical reason baby not eating well.
8. Space out meals from bottle or breastfeeding time.
7. Try, try, and try again (10 times rule).
6. Develop good habits.
5. If you have to, use some tricks like tv time or holding your baby.
4. Camouflage with foods she does like.
3. Let baby play in the food.
2. Eat with your baby, she learns by example. And the #1...
1. Enjoy meal time with your baby!
(To Top)
4. How do I make baby food?
Please refer to the "Baby Food" article.
Making baby food is easy and I mean it! My 3 year old shows how easy in his cooking videos. You don't even need a recipe. When first introducing baby food to your little one it is a single ingredient dish, i.e. pureed sweet potatoes or pureed pears that's it! with just a little water or breast milk/ formula to puree it. For example,
- Peel the skin off of the sweet potato.
- Cook the sweet potato (I like to steam it).
- Puree the sweet potato using the water you used when cooking the potato until you get a good consistency. Some people like to use a blender if they don't have a food processor.
- Put pureed food in an ice cube tray.
- Freeze.
- Once frozen pop out the cubes and store in a container in the freezer.
- Microwave a cube for approximately 30 seconds when ready to serve. (Make sure you stir well to eliminate all of the hot spots.)
(To Top)
5. I read it isn't safe to make my own baby food?
Please refer to the "Baby Food" article.
Some research indicates that you should not make homemade baby food from food such as carrots, squash, spinach, collard greens, beets, turnips, or green beans since they may contain a higher nitrate level and your baby could get blue baby syndrome. According to the American Academy of Pediatrics, if you are making baby food for an infant older than 6 months you should not have to worry about this as by 6 months "babies have enough hydrochloric acid in their tummies to neutralize the nitrates and get rid of them" (Sears, Happy Baby 176).
(To Top)
6. How do I know if my baby has an allergy?
Please refer to the "Introducing Baby Food" article.
Some signs are:
- Spitting up1
- Diarrhea1
- Constipation1
- Blood in the stool1
- Irritability1
- Skin rashes1,2or diaper rash2
- Swelling of face or tongue2
- Congestion such as a stuffy or runny nose lasting more than two weeks2
- Wheezing or rattling in the chest2
- Vomiting2
1Greene,
Feeding 171
2Sears,
Happy Baby 167
Even if your baby is not allergic to the food, your baby could become constipated when you introduce the food as a lot of the first foods can be constipating. If after changing the foods and your baby is still constipated or has very loose stools, "consider the possibility that your baby has a cow's milk protein allergy. It more commonly causes loose stools, but it is also often a cause of constipation" (Greene, Feeding 159). Some babies may experience a food intolerance which is not considered an allergy. According to Sears, symptoms of a food intolerance may be:
- Diarrhea (runny or mucous stools)
- Night waking or fussiness
- Upset stomach, vomiting, gas pains (Happy Baby 167)
(To Top)
7. What may cause an allergic reaction?
Please refer to the "Introducing Baby Food" article.
According to Sears, the foods that account for the 90% of food allergies in children are:
- Cow's milk products
- Egg white
- Fish
- Peanuts
- Shellfish
- Soy
- Tree Nuts (almonds, cashews, and walnuts)
- Wheat (Happy Baby 167 - 168)
A lot of sources recommend waiting until over a year to start the allergy prone foods. Food "such as cheese, yogurt, baby cereals, teething biscuits, breads, egg yolk, mild fish like wild salmon or cod, and tofu" can be started around nine months (Happy Baby 168).
(To Top)
8 . How much should baby be eating?
Please refer to the "How Much to Eat" article.
I compiled information from The Baby Book, babycenter.com, Healthy Sleep Habits, Happy Child, Secrets of the Baby Whisperer, and my personal experience to prepare a table broken out by age of the baby.
| Age |
Total Amount (Ounce) |
Time on Breast
(Minute) |
Bottle Amount
(Ounce) |
# Times Per Day |
Solid Food
(Per Day) |
Additional Notes |
| Birth - 3 Weeks |
12 - 24
|
40
single side |
1 - 2
or 3 |
6 - 12 |
|
Recommended to wake
baby if 3 - 4 hours
passed since last feeding. |
| 1 - 2 Months |
12 - 24
(up to 36 - 40) |
30 - 40
single side |
3 - 4
or 4 - 6 |
6 - 8 |
|
By one month most eat 4 ounces every 4 hours including during the night. |
| 3 - 4 Months |
12 - 24
(up to 36 - 40)
|
Up to 20 single side
|
4 - 6
or 4 - 8 |
6 |
|
By 4 months, usually can sleep six hours straight before waking to eat. |
| 5 - 6 Months |
12 - 36 |
Up to 20 single side
|
4 - 6
or 8 |
4 - 6 |
Start solids, usually starting with baby cereal. |
Around 5 months most start solids. By 5 months usually can sleep nine hours and by 6 months usually can sleep twelve hours before waking to eat. |
| 7 - 8 Months |
24 - 32 |
Up to 20 single side
|
8 |
3 - 5 |
2 - 3 times |
|
| 9 -10 Months |
24 - 32 or
16 - 24 |
Up to 20 single side
|
8 |
3 - 4 |
3 times |
|
| 11 - 12 Months |
24 - 32 or
16 - 24 |
Up to 20 single side
|
8 |
3 - 4 |
3 times |
|
| 12 - 24 Months |
16 - 24 |
Up to 20 single side
|
8 |
3 |
3 times |
Can transition to whole cow's milk (limit to 24 ounces or may obtain iron deficiency); healthy snacks between meals may increase as well. |
(To Top)
9. What if my child is a picky eater?
Please refer to the "Picky Eater" article.
- Set a Good Example
- Make it Fun
- Use Dip
- Let Them Help
- Interrupt Play Time
- Give a Choice
- Put Everything in One Pot
- Keep Trying
- Relax
(To Top)
10. What are good feeding an infant resources?
Please refer to the "Food Resources" article.
(To Top)
11. Where can I find a list of all articles?
Please refer below for a summary or to the Food Home page. Or please refer to the the All Articles Home page.
Infants & Toddlers
(To Top)
1. How much do most babies drink?
Please refer to the
"How Much" article.
Remember, the amount your baby drinks varies baby to baby, but one way to calculate the average amount most babies drink is to use the following equation documented at drgreene.com:
| |
2 or 3
Ounces (oz.) |
Multiply by |
Total Baby Weight in Pounds (lbs) |
Equals |
Total Amount in 24 Hours in Ounces (oz.) up to MAXIMUM 32 oz. |
| Ex. 1 |
2 or 3 oz. |
X |
10 lbs |
= |
20 - 30 ounces |
| Ex. 2 |
2 or 3 oz. |
X |
20 lbs |
= |
32 ounces
(Since MAXIMUM reached) |
I also compiled information based on my interpretation from The Baby Book, babycenter.com, Healthy Sleep Habits, Happy Child, Secrets, and my personal experience to prepare a table broken out by age of the baby to list the total amount, amount per bottle, number of bottles per day, how often to give bottles, and additional notes. Note: How often to give bottles at the beginning may include during the night time. Generally by 6 months, the baby can sleep through the night without waking to sleep and thus the how often only refers to during the day. Please refer to the actual source for more detailed information.
| Age |
Total Amount (Ounce) |
Bottle Amount
(Ounce) |
# Bottles/
D ay |
How Often (Hour) |
Additional Notes |
| Birth - 3 Weeks |
12 - 24
|
1 - 2
or 3 |
6 - 8 |
3 |
Recommended to wake
baby if 3 - 4 hours
passed since last feeding. |
| 1 - 2 Months |
12 - 24
(up to 36 - 40) |
3 - 4
or 4 - 6 |
6 - 8 |
3 - 4 |
By one month most eat 4
ounces every 4 hours
including during the night. |
| 3 - 4 Months |
12 - 24
(up to 36 - 40)
|
4 - 6
or 4 - 8 |
6 |
3 - 4 |
By 4 months, usually
can sleep six hours
straight before waking to
eat. |
| 5 - 6 Months |
12 - 36 |
4 - 6
or 8 |
4 - 5 |
3 - 4 |
Around 5 months most start solids. By
5 months usually can
sleep nine hours and by
6 months usually can
sleep twelve hours before
waking to eat. |
| 7 - 8 Months |
24 - 32 |
8 |
3 - 4 |
4 |
Solid foods 2 - 3 times. |
| 9 -10 Months |
24 - 32 or
16 - 24 |
8 |
3 - 4 |
4 |
Solid foods 3 times. |
| 11 - 12 Months |
24 - 32 or
16 - 24 |
8 |
3 - 4 |
4 |
Solid foods 3 times. |
| 12 - 24 Months |
16 - 24 |
8 |
3 |
4 |
Solid foods 3 times; can
transition to whole cow's
milk (limit to 24 ounces
or may obtain iron
deficiency) |
(To Top)
2. What is the best baby bottle?
Please refer to the "Bottles" article.
This is definitely personal preference for both baby and parents. We tried a lot of different bottles to find one our son preferred. For our son, our favorite bottle was the Dr. Browns since our son seemed to drink well without a lot of air bubbles when using the Dr. Browns. I also liked that Dr. Brown's had glass bottles.
For our daughter, since she preferred breastfeeding, the Tommee Tippee bottles worked best. These seemed to have
a more realistic nipple to compliment breastfeeding. Please refer to the "Nipples" article for more information on types of bottle nipples.
We also liked the Avent wide neck bottles and bottle nipples that helped a baby latch on similar to when she's breastfeeding. The Evenflo bottles didn't work well for us. My son wasn't use to the latex texture of the Playtex nipples used with the Playtex bottles, but for some babies that do well breastfeeding this texture may seem more similar to mom and may help with transition from breastfeeding to bottle feeding.
If you are introducing a bottle early and you want to breastfeed as well you may want to consider using a Haberman bottle.
No matter what bottle you choose I would make sure it is Bisphenol-A (BPA) free although I think most all baby bottles are now made BPA free.
(To Top)
3. What type of formula should I buy?
Please refer to the "Formula" article.
There are many different formulas to choose from: milk based, soy based, or hypoallergenic. In addition, most offer DHA, and some formulas offer probiotics and some are also organic. Most formulas are made with a whey/casein mix. Our favorite formula was Nestle Good Start Protect Plus with Probiotics which was 100% whey. Our son seemed to digest this formula easier than the other formulas.
With my daughter I was planning to use Earth's Best Organic formula but she was solely breastfed so I never offered her any formula.
Unless your child has an allergy I wouldn't jump to the Hypoallergenic formulas or the formulas designed for "fussy" babies. I would confirm with your doctor first. Be aware that for the non milk-based formulas the first ingredient generally listed is corn syrup solids. If you believe your child has a milk allergy (may spit up could be sign of reflux or milk allergy) then you will want to discuss with your doctor and possibly try the hypoallergenic or soy formulas. Some also feel that some babies with eczema do better on organic formulas.
If you start with one formula and need to transition to another, generally it is best to do the transition gradually. Please refer to the "Formula Transition" article for more information.
(To Top)
4. What if my baby won't drink a bottle?
Please refer to the "Feeding Tricks" article.
If this is something new (she previously drank a bottle fine) your child may have reflux. That is what happened to our son.
He was drinking 6 - 8 ounces at a sitting and suddenly around 4 months he became very upset at feedings and would only drink 2 - 3 ounces. If you have a similar problem you will want to discuss with your medical professional so you can identify the problem. Your child could also be allergic to milk. Some babies initially diagnosed with reflux actually had a milk allergy. Some babies may reject the bottle due to teething.
If your child won't drink a bottle because she has nipple confusion and only wants to breastfeed, I would try having someone other than mommy give her a bottle. It may take time. Also, try various bottles and different nipples.
My daughter who preferred breastfeeding would only drink out of Tommee Tippee bottles and the milk had to be very warm. But you could try having the baby latch on and start breastfeeding and then put the bottle in your baby's mouth since she was already sucking she may continue sucking on the bottle.
Some other feeding tricks we had to do with our son was to feed him after he fell asleep. I wouldn't recommend this unless it is the only way to get your child to eat. It was our last resort and it worked great for months when my son didn't want to drink his bottle. We would also feed my son in a calm quiet place with no distractions. (Before my son developed feeding problems we could feed him anywhere.) Due to the reflux, small frequent feeding worked best and so staying on a feeding schedule helped.
(To Top)
5. What if my baby spits up after drinking?
Please refer to the "About Reflux" article for more information.
All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
(To Top)
6. Water used to prepare formula?
Please refer to the "Water" article.
I initially
didn't think about this question, I simple used tap water filtered in our Brita. Later, I read you are suppose to use distilled water. So I started to primarily use distilled water and only about 8 ounces of tap water. I continued to use some tap water so my son would get fluoride in the water but I didn't want to use too much because I didn't want him to develop fluorosis.
(To Top)
7. How should I warm the bottle?
Please refer to the "Bottle" article.
You are not suppose to warm the bottles in the microwave as the milk can get hot spots and burn the baby. We used the Avent bottle warmer which worked for other non-Avent bottles as well. We felt the Avent warmer could have been designed better. For example, when you turn it on to warm the light comes on for about a 2 1/2 minute cycle and then turns off; this does not mean the bottle is actually warm though. We generally waited for it to go through two cycles (about 4 - 5 minutes) if the bottle was cold out of the refrigerator.
Once you do warm the bottle, it is recommended to test the formula or breast milk on your wrist to make sure it is not too hot. For my son, I felt the breast milk or formula was a perfect temperature if I couldn’t feel it on my wrist, meaning it was body temperature. Our daughter liked the bottle on the warmer side. If you heat the bottle too much not only could the bottle break or the formula or milk be too hot for the baby to drink but it may ruin the composition of the milk.
(To Top)
8. How many bottles will I need?
Please refer to the "How Much" article to find out how much the norm baby eats to determine how many bottles you'll need each day.
If you are able to afford it, the more bottles you have the easier. If you are able to buy enough bottles for the entire day and then simply put them in the dishwasher once a day that is ideal. If you get around 8 – 10 bottles generally that should be sufficient.
(To Top)
9. When and how do I wean my baby?
Please refer to the "Weaning from Bottle" article.
Many wean the baby from a bottle by the time the baby is around one year old. The main reason to wean a baby from the bottle earlier than later is as the child approaches the two year mark, it may be harder to wean than when the child is “between twelve and eighteen months” (Sears 215). Although, Sears also discuss that “[i]t is not unusual or abnormal for a baby to still want a bottle at two years of age” (215). In addition, Sears in reference to breastfeeding weaning state, "weaning occurs when the sucking need dissipates - sometime between nine months and three and a half years" (195). It is important to make sure the child does not associate going to sleep with drinking a bottle and instead develops good sleep habits. Please refer to the “Sleep” section for more information. Another reason to wean from bottle feeding is to avoid tooth decay and an overbite.
When it is time to wean, you may transition your child to a sippy cup or straw cup. It may help to have your child pick up his new special cup.
(To Top)
10. Eliminate the middle of the night bottle?
Please refer to the "Nighttime Weaning"article or the "Nighttime Parenting" article.
In general, most research recommends you can wean the baby from night feeding between 6 - 9 months. According to Weissbluth, in the sleep maturation process by nine months there is no longer night waking for a feeding (15). According to the Disney article, most babies can sleep without waking to eat according to the following schedule:
| Age |
Time Before Waking to Eat |
| 3 weeks - 4 months |
Range (2 - 6 hours) |
| 4 months |
6 hours |
| 5 months |
9 hours |
| 6 months |
12 hours |
Remember, that the above schedule is the "norm" for most babies. Each baby is an individual and if "your child was a preemie or has acid reflux, he'll likely need to eat more often..." (Disney). For my family with my son because he had reflux and didn't eat a lot during the day I definitively wanted to feed him in the middle of the night when he would wake up and want to eat. For my daughter, even though she ate fairly well during the day when she would wake in the middle of the night it was easiest for me to simply feed her and then she would immediately go back to sleep.
(To Top)
11.What are good bottle feeding resources?
Please refer to the "Breastfeeding & Bottle Feeding Resources" article.
(To Top)
12. Where can I find a list of all articles?
Please refer below for a summary or to the Breastfeeding & Bottle Feeding Home page. Or please refer to the the All Articles Home page.
Infants & Toddlers
(To Top)
1. Should I breastfeed my baby?
Please refer to the
"To or Not To?" article.
To breastfeed or not to breastfeed is definitely a personal question you have to answer yourself. There are many different studies out there and a lot of the research does tend to promote breastfeeding; but ultimately you have to do what works best for you and your family.
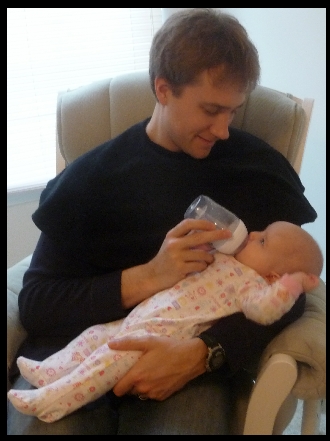
Breastfeeding does offer the baby immune support and other health benefits, may help both mom and baby relax, may save time (or could increase the amount of time), may help with postpartum recovery, has health benefits for mom (may help lose baby weight), and can save money. For my daughter, I solely breastfed her (Daddy would give an occasional bottle) and it was a wonderful bonding experience for both of us. For my son, breastfeeding was not as natural as with my daughter and I enjoyed giving my son a bottle. If you bottle feed along with breastfeeding it does allow your spouse to share in the feeding process and may give more flexibility but you will have to make sure you pump every time someone gives your baby a bottle or you won't produce enough breast milk. If you don't you will have to supplement with formula, which that is fine if that is what you want to do.
You can breastfeed and bottle feed your baby. For me giving my son formula as well as breast milk worked and for my daughter I preferred breastfeeding and so we gave her very little bottles and she never had to have any formula. Ultimately, you have to decide what works best for you and your family.
(To Top)
2. How long and how often to breastfeed?
Please refer to the "How Much" article.
Breastfeeding is definitely going to vary baby to baby. Not only is there the baby differential, but mommy impacts this one as well since not all women produce and distribute breast milk the same. Most research advises against watching the clock while breastfeeding. I definitely agree that you do not want to be concerned with the exact time the baby breastfeeds and that ultimately you have to feed your baby according to your baby’s needs. On the other hand, I also feel it is also nice to have a rough idea of the “norm” times for breastfeeding.
Similar to the table for bottle feeding, I compiled information based on my interpretation from The Baby Book, babycenter.com, Healthy Sleep Habits, Happy Child, Secrets, and my personal experience to prepare a table to list the time on breast, the amount, number of times breastfeed, how often, the total amount, and additional notes about breastfeeding. Please refer to the actual source for more detailed information.
| Age |
Time on Breast (Minute) |
Amount
(Ounce) |
# Breast |
How Often (Hour) |
Total Amount (Ounce) |
Additional Notes |
| Day 1 |
5 on each side |
|
8 - 12 |
On demand |
12 - 24 |
Some feed every 1 1/2
hours, others every 3
hours. Recommended to
wake baby if 3 - 4 hours
passed since last feeding. |
| Day 2 |
10 on each side |
|
8 - 12 |
2 |
12 - 24 |
|
| Day 3 |
15 on each side |
|
8 - 12 |
2 1/2 |
12 - 24 |
|
| Day 4 - 3 Weeks |
40 single side |
|
8 - 12 |
2 1/2 - 3 |
12 - 24 |
|
| 1 Month |
Up to 40 single side
|
2 - 5
|
8 |
3 |
12 - 24
(up to 36 - 40) |
By one month most eat 4 ounces ever 4 hours including during the night. |
| 2 Months |
Up to 30 single side |
4 - 6 |
6 - 8 |
3 |
12 - 24
(up to 36 - 40) |
|
| 3 - 6 Months |
Up to 20 single side
|
5 - 8 |
6 |
3 |
12 - 24
(up to 36 - 40) |
By 4 months, usually
can sleep six hours
straight before waking to
eat. Around 5 months most start solids. By
5 months usually can
sleep nine hours and by
6 months usually can
sleep twelve hours before
waking to eat. |
| 7 - 8 Months |
Up to 20 single side |
8 |
4 - 5 |
4 |
24 - 32 |
Solid foods 2 - 3 times. |
| 9 -10 Months |
Up to 20 single side |
8 |
3 - 4 |
4 |
24 - 32 or
16 - 24 |
Solid foods 3 times. |
| 11 - 12 Months |
Up to 20 single side |
8 |
3 - 4 |
4 |
24 - 32 or
16 - 24 |
Solid foods 3 times. |
| 12 - 24 Months |
Up to 20 single side |
8 |
3 |
4 |
16 - 24 |
Solid foods 3 times; can
transition to whole cow's
milk (limit to 24 ounces
or may obtain iron
deficiency) |
(To Top)
3. Is baby getting enough breast milk?
Please refer to the "How Much" article.
Since breastfeeding does not give you the exact amount the baby is drinking, I was always wondering if my son was getting enough milk. This was my main concern and a contributing factor as to why I liked to occasionally give my son a bottle to see how much he would drink from the bottle. With my daughter I was more comfortable with breastfeeding and I knew she was getting enough milk: I could hear her gulping the milk, when I did pump I had a lot of it; when she would occasionally take a bottle she would easily drink the "norm" amounts so I knew if she wasn't getting that same amount when I breastfed her she would have been crying.
If you would like to obtain an estimate of what your breasts provide your baby then “fifteen minutes before a feed, pump your breasts and measure what you are yielding. Taking into account that a baby can extract at least one ounce more by physically sucking at your breast…” (Hogg 108).
If you do not want to occasionally give your baby a bottle or pump to find out, how do you know your baby is drinking enough? Well, you may not know exactly but there are signs to look for such as how many wet diapers or bowel movements the baby has. I compiled information from both La Leche League (LLLI) "Milk" article and Sears (pages 99 &139) to prepare the table below.
| |
Wet Diapers
(Disposable) |
Bowel Movements |
Additional Notes |
Day 1 & 2
(Only Colostrum in Breast Milk) |
1 or 2 |
|
If bottle feeding, I would expect more wet diapers day 1 and day 2. |
| Around Day 4 - 1st Few Months |
4 - 6 |
2 - 5 |
Some babies may only have 1 or 2 bowel movements a day. Some babies start having less frequent but large bowel movements around 6 weeks. |
(To Top)
4. Should I switch sides when breastfeeding?
Please refer to the "About Breastfeeding" article.
There is contradictory information relating to whether you should switch sides, from right breast to left breast while breastfeeding. According to Hogg, if you switch sides after ten minutes then the baby won’t be able to get all three components of breast milk, quencher, foremilk and hind milk. “If you switch sides after the first ten minutes, at best your baby is only starting to get foremilk and never gets to the hind milk. Even worse, this switching eventually sends a message to your body that it’s not necessary to produce hind milk” (106).
(To Top)
5. What if my baby won't breastfeed?
Please refer to the "Breastfeeding Tips" article.
The most important advice, I can offer is to seek help. With my son I was embarrassed and didn't get enough advice from the lactation consultants prior to leaving the hospital and I didn't want to schedule a follow-up visit. With my daughter I saw them every day I was in the hospital (and I was there five days) and although it still took some time adjusting the first month it became a natural process and it worked well for both of us. Refer to Breastfeeding & Bottle Feeding Resources, for more resources such as La Leche League International or the U.S. Department of Health & Human Services that offer advice about breastfeeding.
You may want to seek advice from other moms as well. Please don't hesitate to post information to the Breastfeeding Community page.
(To Top)
6.What if my baby spits up after nursing?
Please refer to the "About Reflux" article for more information.
All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
(To Top)
7. How do I store extra breast milk?
Please refer to the "Storing" article.
Breast milk can be stored for a short period at room temperature, in the refrigerator, or in the freezer and sources differ on how long you can keep breast milk. Please refer below for guidelines according to the La Leche League International (LLLI "Storing").
| Type |
Amount of Time |
Temperature |
| Room Temperature |
4 (ideal) - 6 hours (acceptable) |
66 to 78°F |
| Refrigerator |
72 hours (ideal) up to 8 days (acceptable) |
<39°F |
Thawed Milk
(Previously Frozen) |
24 hours in the refrigerator (do not re-freeze it) |
<39°F |
| Freezer |
6 months (ideal) up to 12 months (acceptable)1 |
-0.4 to -4°F |
1If you do freeze the breast milk, even though according to the LLLI you can keep the milk up to 12 months you may not want to keep the milk longer than six months. Your body produces a different type of milk early in the baby’s life versus later so you would not want to give a nine month old baby breast milk you pumped when he was three months old. According to Eiger, “[i]t’s best to use milk soon after collecting it. Ideally, you will not keep it longer than three months.” In addition it is not good to freeze the breast milk for an extended period of time since “long-term freezing alters the chemical composition of the milk” (Eiger 351).
(To Top)
8. What are some accessories I need?
Please refer to the "Breastfeeding Accessories" article.
Some accessories you may want to get would be:
(To Top)
9. What's in breast milk?
Please refer to the "About Breastfeeding" article.
I noticed that the breast milk would separate into different parts. According to Hogg, the different layers you see is also how it is delivered to your baby,
Quencher (first five to ten minutes): This is more like skim milk…satisfies Baby’s thirst. It’s rich in oxytocin....[and] also has the highest concentration of lactose.
Foremilk (starts five to eight minutes into the feed): More like the consistency of regular milk, foremilk has a high protein content, which is good for bones and brain development.
Hind milk (starts fifteen or eighteen minutes into the feed): This is thick and creamy, and it’s where all the goody-goody fat is – the “dessert” that helps your baby put on weight (106).
(To Top)
10. What is the let-down reflux?
Please refer to the "About Breastfeeding" article.
The let-down reflex “is a hormonally driven process that gets the milk from the upper portions of the breast through the ducts to the sinuses beneath the areola, out the nipple and finally into a baby’s waiting mouth” (Vickers). But how do you know if your breasts have let-down and the baby is getting breast milk? “THE BREASTFEEDING ANSWER BOOK goes on to say that the ‘most reliable sign of the let-down is a change in the baby’s sucking and swallowing pattern from quick sucks with occasional swallowing to long, slow sucks with regular swallowing or gulping’….Some women barely feel any let-downs, while others experience a tingly sensation in the breast every time the milk lets down” (Vickers).
(To Top)
11. How can I get my baby to latch on?
Please refer to the "About Breastfeeding" article.
You may have heard about the problem of sore nipples when breastfeeding. In general, the main solution to prevent sore nipples or (cracked nipples) is to make sure the baby latches on correctly. The following are some tips based on my personal experience in addition to those I read in the "Position" article at the LLLI’s web site:
- Make sure you’re comfortable. Sit in your comfort chair, ideally with your feet supported by a footrest and position the baby in your lap. You may want to use a Boppy Pillow or regular pillows to support the baby.
- Position baby by making sure “he does not have to turn his head to reach your breast. His mouth and nose should be facing your nipple.”
- “Support your breast.”
- Help baby latch on. My sister-in-law told me how you can rub the baby’s bottom lip (with your nipple or finger) and it usually encourages the baby to open his mouth. It is important to bring the baby to you and not your breast to the baby. I know sometimes I would do the opposite and it can be uncomfortable trying to lean into the baby rather than sitting comfortably and bringing the baby to you (“Position”).
(To Top)
12. How can I increase my milk supply?
Please refer to the "About Breastfeeding" article.
It is important to remember that primarily “milk production is based on supply and demand—how much milk the breast makes is determined by how much milk is removed from the breast” (Vickers). Although, some women may produce a ton of milk while others have to work at it. You may not be sure how much milk your producing, so one way to find out is fifteen minutes before you breastfeed, pump your breasts and measure what you are yielding. “Taking into account that a baby can extract at least one ounce more by physically sucking at your breast…” (Hogg 108).
If you don’t feel your producing enough milk then it is usually recommended to allow baby to be placed on each breast at each feeding. Remember to let the baby primarily finish feeding on one side so he can receive the hind milk before switching to the other side. In this case you are primarily only switching the baby to the other side to stimulate the breast so it can produce more milk.
Some other tips to produce more milk are to sleep, drink water, and pump.
(To Top)
13. Can I exercise if I breastfeed my baby?
Please refer to the "About Breastfeeding" article.
Exercise is definitely good for the body. Trying to find time in the day when you have a little one may not be easy. In addition, if you are breastfeeding you may want to pay attention to when you exercise. According to Eiger, it is best to exercise after you breastfeed the baby. If you do strenuous exercise then your breast milk may taste differently to the baby due to a short-term rise in lactic acid concentration. “Lactic acid levels are less likely to rise after moderate exercise, and in any case are not harmful to infants.” It is also important to drink extra water when exercising since you’ll need to replenish any fluid lost while exercising (150-151).
(To Top)
14. When and how do I wean my baby?
Please refer to the "Weaning from Breastfeeding" article.
Most professionals, including the Acting Surgeon General, Steven K. Galson, suggest breastfeeding is best. According to the U.S. Surgeon General’s public health report, “health professional organizations… officially recommend that most infants breastfeed for at least 12 months. These organizations also recommend that for the first six months infants be exclusively breastfed, meaning that they not be given foods or liquids other than breast milk” (356).
Many women wean around the time the child is over a year and thus simply transition to whole cow’s milk in a sippy cup.
If you are trying to wean from breastfeeding to formula feeding, the Gerber web site has a sample schedule, please refer to this link. The schedule states to try the following assuming eight feedings a day.
- Day 1, 2, 3 switch out one feeding with formula.
- Day 4 and 5 switch out two feedings with formula.
- Day 6 and 7 switch out three feedings.
- Day 8 and 9 switch out four feedings.
- Day 10 and 11 switch out five feedings.
- Day 12 switch out six feedings.
- Day 13 switch out seven feedings.
- Day 14 switch out all feedings.
If the baby rejects formula you may try mixing it with breast milk.
(To Top)
15. Eliminate the middle of the night feeding?
Please refer to the "Nighttime Weaning"article or the "Nighttime Parenting" article.
In general, most research recommends you can wean the baby from night feeding between 6 - 9 months. According to Weissbluth, in the sleep maturation process by nine months there is no longer night waking for a feeding (15). According to the Disney article, most babies can sleep without waking to eat according to the following schedule:
| Age |
Time Before Waking to Eat |
| 3 weeks - 4 months |
Range (2 - 6 hours) |
| 4 months |
6 hours |
| 5 months |
9 hours |
| 6 months |
12 hours |
Remember, that the above schedule is the "norm" for most babies. Each baby is an individual and if "your child was a preemie or has acid reflux, he'll likely need to eat more often..." (Disney). For my family with my son because he had reflux and didn't eat a lot during the day I definitively wanted to feed him in the middle of the night when he would wake up and want to eat. For my daughter, even though she ate fairly well during the day when she would wake in the middle of the night it was easiest for me to simply feed her and then she would immediately go back to sleep.
(To Top)
16.What are good nursing resources?
Please refer to the "Breastfeeding & Bottle Feeding Resources" article.
(To Top)
17. Where can I find a list of all articles?
Please refer below for a summary or to the Breastfeeding & Bottle Feeding Home page. Or please refer to the the All Articles Home page.
Infants & Toddlers
(To Top)
Please refer to the Community Home page for a list of all community articles or the All Articles Home page.
1. Do I really need to serve organic food?
Please refer to the
"Organic" article.
I believe the greatest gift you can give your family is the gift of health! I believe one way to give the gift of health is to truly know what you are feeding your family, look at the ingredients in products you are buying and try to buy organic to avoid pesticides, artificial hormones, antibiotics, genetically modified organisms, artificial colors and preservatives, and added nitrates.
(To Top)
2. I can't afford to buy organic?
Please refer to the "Organic" article.
I understand that buying organic can cost more. I understand that some people simply cannot afford it. But I do feel that others do not want to afford it. If you can provide your child the latest toy or you get your hair done at a nice hair salon or you just bought a new outfit because you wanted to then I would expect you can give your child the greatest gift, the gift of health. (I can't guarantee your child will be healthy if she eats organic, all I can tell you is I feel it is the best food for my family.)
If you factor in the fact you receive more vitamins, minerals, and nutrients and avoid "exposure to pesticides, which are known to kill brain cells and cause cancer in laboratory studies" and overall are providing more nutritious food to your family [and hopefully avoiding cost of unnecessary medical care] I think you are actually saving money (Sears, Happy 193).
My personal experience, I'm actually spending less out of pocket once I started shopping at Whole Foods and buying almost all organic food. Why? The first reason is that I'm decreasing the amount of pre-packaged food items. Have you ever looked at what are the more expensive items on your grocery bill? It usually isn't the bag of apples it is the box of cookies or some other pre-packaged item. The second reason I'm spending less is by shopping at a place like Whole Foods, that has a slogan of "Selling The Highest Quality Natural & Organic Products"; I feel the organic products are cheaper there than than buying organic at a standard grocery store that carries some organic products. In addition, Whole Foods has specials each week so I buy whatever meat is on special that week.
Overall, I understand that buying organic may not be a viable option for everyone, which is why I like the following quote: “[b]uy the best you can afford. This will reduce your exposure to pesticides, hormones, and other toxins” (McCarthy 266). You may want to at least buy organic for some of the important foods to avoid.
If you are unable to buy organic products either you don't have access to them or simply can't afford them then I urge you to limit your packaged food items. You will save money and serve better food for your family.
(To Top)
3. How do you go shopping with kids?
Please refer to the "Grocery List" article.
Grocery shopping with kids is definitely a different experience than shopping by yourself. It truly is a treat when I get to shop by myself. It is fun watching my 3 year old push his own cart or my 9 month old smile at people but definitely easier to simply shop by myself. That said, I rarely have the opportunity to shop by myself so here are a few tips:
- Be Organized - Bring your list using a template to help you find your items as quickly as possible
- Bring Snacks (I end up opening some of the food that I intend to buy.)
- Wear Your Baby
- Make it Fun & Let Them Help
(To Top)
4. What are some healthy snacks?
Please refer to the "Healthy Snacks" article.
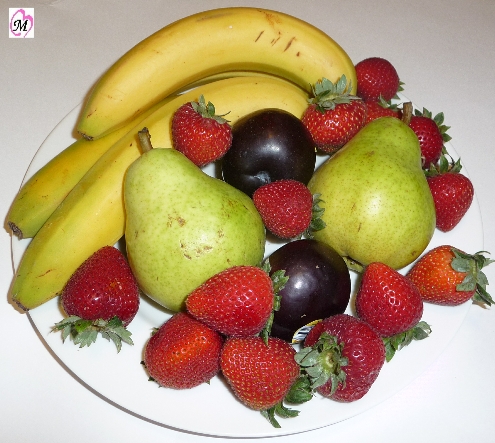
My favorites are (I serve the organic version):
- Cereal
- Cheese sticks
- Animal Crackers/ Graham Crackers/ Fig Cookies
- Dried Fruit
- 100% Juice (No Sugar Added), Chocolate Milk, Almond Milk, or PediaSmart
- Fruit/ Homemade Fruit Cup
- Homemade Treat
- Peanut Butter Crackers
- Homemade Popcorn (NOT Microwave popcorn that contains chemicals)
- Smoothies
- Yogurt
(To Top)
5. What are your favorite meal ideas?
Please refer to the "Dinner Meal Ideas" article.
I personally like anything that is quick and easy. I love to make things that you can make in one pot such as homemade chicken noodle soup (super easy), anything in the crock pot such as a mushroom/onion roast, or something in a casserole dish such as chicken goop. (Recipes coming soon)
(To Top)
6. What are good food resources?
Please refer to the "Food Resources" article.
(To Top)
7. Where can I find a list of all articles?
Please refer below for a summary or to Food Home page. Or please refer to the the All Articles Home page.
All
Infants & Toddlers
(To Top)
1. My baby cries all of the time. Is It colic?
Please refer to the "Crying Baby...Is It Colic" article.
Remember that all babies cry. “The average 6-week-old fusses or cries more than an hour a day. A full 25% cry more than two hours" (CDHNF). So how do you know if your baby is crying the normal amount of time or if your baby is "colicky" or a "hurting baby?" In general:
- " 20 percent of babies suffer from some form of colic"
- Of the 20%, "10 percent are considered severe cases” (Hogg 263).
One way to decide if your baby is a true "colic" or "hurting baby" is to follow the "rule of three"
- last at least three hours a day, occur three days per week, and continue for at least three weeks
- begin within the first three weeks of life
- seldom last longer than three months
- occur in an otherwise healthy, thriving baby (Sears 384)
As described by Sears, some babies may be colicky only in the evening and unfortunately others may be colicky all day. For the evening-only colicky babies, they are usually very happy during the day and people would never know that they are considered colicky at night and these babies tend to sleep well at night. The good news with the evening only colicky babies, generally, “there is rarely an underlying medical cause...” (Sears 384). Based on my mommy instinct, I would think for some of these babies they are simply over exhausted from the day and are having trouble settling down for the night. My son was not colicky but he definitely would have more "fussy" periods at night when he was tired.
On the other hand, the all-day colic baby “is rarely happy” and "[h]e spends most of the day fussing, squirming, or screaming.” In addition, these all day colic babies are usually restless sleepers. This is where the Sears state this baby deserves the "hurting baby" title (Sears 384). My heart goes out to both the babies and the caregivers for these babies.
(To Top)
2. Baby wakes up sick in middle of night?
Please refer to the "Sick in Middle of Night" article for more information.
If it is an emergency you should call 911 but most of the time it is something you are concerned about but not an emergency. Most pediatricians give you a number you can call (even if it is the middle of the night) if you are concerned about your baby. If you are unable to reach your child's doctor you could call your local pharmacy to discuss symptoms and they may be able to give some general advice. Most health insurance has a 24 hour nurse's line, check on the back of your insurance card. I would ere on the side of caution and seek help if you are concerned about your baby. Trust your instinct and follow-up if you think something is wrong.
(To Top)
3. What if my baby spits up all of the time?
Please refer to the "About Reflux" article for more information.
All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
(To Top)
4. What is infant reflux?
Please refer to the "About Reflux" article for more information.
According to Children’s Digestive Health and Nutrition Foundation, (CDHNF) “Gastroesophageal Reflux occurs when an infant’s muscular sphincter-- where the esophagus enters the stomach-- allows acidic, gastric (stomach) fluids to reflux, or flow backwards up into the esophagus and sometimes reach as high as the mouth or nose” (CDHNF, "Coping"). All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
The following are some facts about reflux and GERD:
- "The majority of infants do not experience problems from reflux"1
- "More than 50% of babies spit up regularly in the first months of life"1
- "Reflux usually peaks at 4 months and stops by 12 – 18 months"1
- "Spitting up crosses the line into GERD when the infant begins to show symptoms including refusal to feed, poor weight gain, breathing problems and others."1
- "[R]eflux (GER) and cow milk allergy (CMA) occur frequently in infants younger than 1 year....up to half of cases of GER in infants...may be an association with CMA....[and] also CMA induced."3
- Reflux is "[o]ne of the most common hidden medical causes of nightwaking (and colicky behavior)...."4
- "In many cases GERD in kids can be managed with lifestyle changes, and without medication"1
- "GERD often runs in families"1
- "Kids with GERD may have frequent complaints of abdominal pain or a tummy ache"1
- "Children and teens with asthma are more likely to have GERD"2
1CDHNF, "Quick Facts about Reflux and GERD"
2CDHNF, "Pediatric"
3Salvatore
4Sears, "31 Ways"
(To Top)
5. What are some symptoms of infant reflux?
Please refer to the "About Reflux" article for more information.
Refer below for a list which compiles the symptoms of GERD. I obtained the description of symptoms primarily from the CDHNF web site.
- Crying – "arching away from breast/bottle with crying or irritability"1,2
- Frequent spitting up (although not all babies with GER spit up regularly)2,3
- "Feeding difficulties1,2
- Feeding refusal1,2
- Poor growth or failure to thrive1
- Difficulty eating (e.g., choking or gagging with feeds)"1,2
- "[P]ainful bursts of nighttime fussiness"2,3
- "[F]requent bouts of colicky, abdominal pain"2,3
- "Breathing problems"1
- "Repeat bouts of pneumonia"1
- "Breathing stops"1
- "Turning blue"1
- "Chronic coughing"1,2
- "Wheezing"1,3
- "[T]hroaty sounds" after feeding3
- "Vomiting associated with"1
- "Blood (e.g., bright red streaks, blood clots or coffee ground appearance in stomach fluids)"1
- "Green or yellow fluid"1
- "Poor weight gain"1
- Projectile vomiting2,4
- Hiccups2
- Spitting up milk through nose2
1CDHNF, "Parent's"
2My son's symptom. Note: Hiccups and spitting up milk though nose was not found as a symptom in medical research, this was my personal experience with my son. This may not be a true symptom of reflux although when we tried to wean my son from his reflux medication I noticed he started getting hiccups again. For my son, there tends to be a correlation between hiccups and when his acid reflux acts up.
3Sears, "31 Ways"
4My son's original doctor told us to look out for reflux when my son was 4 months old by watching for projectile vomiting. At 4 months although my son was refusing to eat he was not projectile vomiting. Not all babies with reflux projectile vomit and as discussed by Sears ("31 Ways") some may not even spit up a lot.
(To Top)
6. What can you do for infant reflux?
Please refer to the "About Reflux" article for more information.
Your pediatrician may recommend a trial of medication that decreases acid in your baby's stomach or refer you to a GI specialist. Our son was put on medication when he was six months old and was on it until about 2 1/2 when he finally seemed to grow out of his reflux. Before my son turned 2 1/2 we tried taking him off the medication several times but he usually would stop eating well and become "needy" when he was usually very independent. When my son was around 2 years old at a visit to the GI specialist she increased his medication as she said the most important thing is to make sure his esophagus is not damaged by the acid. Please refer to the "Medication" article for more information.
If the GERD is extreme then surgery may be recommended. There are also "lifestyle adjustments" that can help a baby:
- "Avoid overfeeding"1
- "Don't feed the baby again after he or she spits up (wait until the next feeding time)"1
- "Check with your doctor to see if you are using appropriately sized bottles or nursing the appropriate amount of time"1
- Our baby drank best with the Dr. Brown's bottles."
- Feed half as much twice as often."2
- Starting at 4 months, our baby would only drink a few ounces at a sitting and so we had to do frequent feedings to help ensure he drank enough for the day.
- "Feeding frequently stimulates more saliva production...[and] [s]alivia contains a healing substance...which helps repair the damaged tissues in the esophagus. It also neutralizes stomach acid and lubricates the irritated lining of the esophagus."2
- If possible, breastfeed your baby
- "[E]asy-in, easy-out" since it empties from the stomach faster and usually produces "softer and easier-to-pass stools"2
- "Breast milk is more intestine friendly than formula."2
- I was able to breastfeed my baby until around 6 months and had I known breast milk would have helped his reflux I would have tried to breastfeed longer. Unfortunately, my son's reflux contributed to weaning from breastfeeding early since around 4 months he didn't want to breastfeed (or bottle feed) and so I started doing more bottles so I could track what he was drinking for the day.
- "If your baby is formula-fed, thicken the formula with a small amount of rice cereal"1
- We switched to oatmeal cereal as it was not as constipating as rice cereal was for our baby.
- Try different formulas, our baby digested Nestle Good Start better than other formulas since it was 100% whey rather than the whey/casein mix of most formulas.
- You may want to try a Hypoallergenic formula to see if your baby has a cow milk allergy.
- Make sure you burp baby well as excess "air aggravates reflux"2
- For awhile, we were hesitant with burping our baby since he got so upset when we burped him but really that was the best thing for him. We found that if we gave him his pacifier when we were burping him that it helped.
- Try other bottles to help minimize air intake or make sure baby is properly latched on for breastfeeding.
- "Keep the baby upright for at least 30 minutes after a feeding."1
- Wear your baby to help keep her upright; I think this helped my baby for the first few months.
- Try to not "jostle or vigorously play with baby after feedings"2 I still try to remind our son's Daddy to try to not play too much right after our son (now almost two years old) eats but that is hard for both him and my son to follow.
- Discuss with your doctor about positioning the baby at night to sleep. It is recommended to put the baby to sleep on her back to help avoid SIDS (Sudden Infant Death Syndrome) but if your baby is suffering from reflux you may want to discuss other sleep positions.
- We elevated our baby's mattress. You can also buy sleep positioners some of which are elevated for the baby. We should have bought one of these.
- "Try not to let your baby spend too much time in a car seat (The baby's position in the car seat can promote reflux)"1
- "Avoid tight diapers and elastic waistbands"1
- Develop parenting style to promote attachment parenting to help decrease crying, "since crying puts pressure on the stomach which worsens the reflux"2
- Pacifier use may help since "sucking stimulates saliva production"2 unless the baby sucks too hard and swallows air then the air can make the reflux worse.
- My son always loved his pacifier and I was happy to let him use something that made him feel better.
- My son is almost two and I still let him have his pacifier for nap and bedtime. I plan to wean in the next year although since he is still suffering from reflux I'm reluctant to wean him. My son's pediatric dentist said we should try to wean him before he turns four. I don't think we should have a problem with that.
- Help baby avoid constipation since "increasing abdominal pressure...can aggravate reflux"2
- Unfortunately, my son had constipation for most of his first year which probably didn't help his reflux.
- Oatmeal cereal was less constipating than rice cereal
- When starting baby food, make sure you avoid or limit the constipating foods like bananas, carrots, and applesauce.
- The "Constipation" article is coming soon
1CDHNF, "GERD in Infants: Treatment and Management"
2Sears, The Baby Book 392 - 397
(To Top)
7. What type of reflux medication is used?
Please refer to the "Reflux Medication" article for more information.
Remember to not give your child any medication that is not prescribed by a doctor, including the over-the- counter (OTC) antacids. Please refer to the following table for a brief description of some common medications. Also, please refer below for some side effects of some of the medications.
| Type |
Description |
Medication Examples |
| 1. Antacid |
These "neutralize stomach acids." Given several times a day (based on your doctor's advice) these work "rapidly, but the neutralizing effects lasts only a couple of hours or less...Long-term use...can contribute to constipation or diarrhea."1 In addition, refer below for more information on possible aluminum toxicity related to antacids. |
Over-the-counter medicines. |
| 2. Acid Suppressor or Reducer |
"Gastric acidity (GA) inhibitors, including histamine-2 receptor antagonists (H2 blockers) and proton pump inhibitors (PPIs), are the mainstay of gastroesophageal reflux disease (GERD) treatment."2 |
|
A. Histamine-2 Receptor Antagonists
(H2 Blockers) |
These "decrease acid production in the stomach....They do not decrease the reflux itself, but make the sloshed liquid less acidic, and thus less likely to cause irritation."3 |
Ranitidine (Zantac);4
Famotidine (Pepcid)4
|
| B. Proton Pump Inhibitors (PPIs) |
These are "powerful at blocking acid production."3 |
Lansoprazole (Prevacid);5 Omeprazole (Prilosec)5 |
| 3. Prokinetic Medications |
These are "supposed to help speed along whatever is in the stomach, and to tighten the valve at the top of the stomach so acid is less likely to slosh up."3 |
Bethanechol (Urecholine); Metoclopramide (Reglan); Antibiotic (Erythromycin)6 |
1Sears 395
2Canani
3Greene
4According to Greene, Zantac and Pepcid "are now approved for children, even infants [one month and older]." Other H2 Blockers like Tagamet and Axid are not approved by the FDA for children under 16 and 12 respectively (April 1, 2008). Please refer below for Zantac product information.
5According to Greene, Prevacid and Prilosec "are newly approved by the FDA for use in children as young as 1 year old." Other PPIs such as Protonix and Aciphex "are not approved by the FDA for use in children. Nexium is not approved by the FDA for use under 12 years" (April 1, 2008). Please refer below for Prevacid product information.
6According to Greene, "[u]recholine has not been approved by the FDA for use in children. Nor has Reglan been approved for use in children, in fact caution is strongly recommended because of increased risk of neurological side effects in children. Erythromycin has been approved by the FDA for children, but not for treating reflux in them."
Generally, Histamine-2 Receptor Antagonists (H2 Blockers) like Zantac are "the first to be used in babies with reflux" since "there has been a lot of experience with these medications." In addition, according to Greene, Ranitidine (Zantac) and Famotidine (Pepcid) are "now approved for children, even infants...." When we met with our pediatrician when my son was 6 months old she recommended starting him on Zantac and if we didn't seem much improvement to then try a Proton Pump Inhibitor (PPIs) like Prevacid.
I had read that Prevacid, although stronger can be more effective, and I didn't see a lot of improvements for my son when he was on the Zantac so we changed to Prevacid. I also discussed medications with a local pharmacist and he said the majority of his pediatric patients were taking Prevacid. I was not happy that Prevacid was not FDA approved for children under 1 years old and I discussed my concerns with our doctor. She said she obviously can't guarantee that it is safe but that infants have been taking the medication and she feels confident in prescribing it for my son. After starting the medication within a week or so, my son was eating his baby food again, when before starting the medication he would clamp his mouth shut and shake his head back and forth when he saw the spoon; definitely not the happy baby with his mouth wide open for baby food. He still didn't drink a bottle as well as he did before he turned 4 months and became a "fussy bottle drinker" but he did seem to drink it better than before we started the medication.
When we saw a GI Specialist, she kept my son on the Prevacid but did increase the dosage. Your doctor may prefer a different medication rather than Prevacid. It seems to vary doctor to doctor. I also know of some infants/ children that take both Zantac and Prevacid. My son seems to do very well on Prevacid alone so I'm happy I don't have to give him another medication on top of that.
(To Top)
8. Are the reflux medications safe for babies?
Please refer to the "Reflux Medication" article for more information.
A lot of the medication prescribed to treat infant reflux is not approved by the FDA, at least not approved for children under one year. Ranitidine (Zantac) and Famotidine (Pepcid) according to Greene, are "now approved for children, even infants...." While Prevacid and Prilosec "are newly approved by the FDA for use in children as young as 1 year old" (Greene). We started my son on Prevacid when he was 6 months old so technically the medication was not approved for children his age. I was surprised to find this out on my own, the doctor when prescribing the medication did not tell me the drug was not FDA approved for a child my age.
"Pediatricians routinely use many drugs which are not FDA approved for a particular use or patient population. Often, this is because the drugs have never been systematically studied in children, not because they are known to be especially dangerous to children" (Greene). On the other hand, if the drug hasn't been tested then the "[s]afety and effectiveness in children have not been established" (Greene). After coming to terms that I didn't really have an alternative and receiving reassurance from my doctor I decided giving my son the Prevacid was the best option for him.
I was also concerned about the "large" dose prescribed to give my baby, initially it was 15mg per day for a six month old baby. I read that adults may take a dose of 15-30mg a day so I didn't understand why I would give the same dose to my baby. Based on some research, I found that "PPI's are less weight sensitive then other meds, so doses will depend on symptoms" (McMahon). I also confirmed with my pharmacist that his other patients were taking a similar dosage.
As with any medication, there are potential side effects. Please refer above for more information on the types of medications and descriptions of those medications.
| Type |
Pro |
Side Effects |
Other |
| Zantac |
"Well tolerated by most children...lots of experience with these medications...usually the first to be used in babies with reflux."1 |
"Headaches, sometimes severe...heart rhythm abnormalities, can be caused by any medicine in this class - but they are quite rare."1 Other side effects are diarrhea and constipation.2 |
Approved for infants one month and older3 |
| (Prilosec/ Prevacid) |
"[M}ore powerful at blocking acid production...."1 and they "are fairly well tolerated...."2 |
"[M]ost common side effects are nausea, diarrhea, constipation, headache, and skin rash"2 |
"[A]pproved by FDA for use in children as young as 1 year old."4 |
| Antacid |
Greene prefers magnesium to aluminum antacids if "it is absolutely necessary to use one of these...."1 |
Possible aluminum toxicity. "The safety of antacids containing aluminum should not be assumed and they should be used judiciously in infants, with careful monitoring of the aluminum dose and plasma level." Other side effects include diarrhea or constipation.5 |
Over the counter |
| |
|
|
|
1Greene (April 1, 2008).
2AAFP
3According to the Zantac Prescribing Information - the "safety and effectiveness of ZANTAC have been established in the age-group of 1 month to 16 years for the treatment of duodenal and gastric ulcers, gastroesophageal reflux disease and erosive esophagitis, and the maintenance of healed duodenal and gastric ulcer. Use of ZANTAC in this age-group is supported by adequate and well-controlled studies in adults, as well as additional pharmacokinetic data in pediatric patients and an analysis of the published literature…Safety and effectiveness in pediatric patients for the treatment of pathological hypersecretory conditions or the maintenance of healing of erosive esophagitis have not been established. Safety and effectiveness in neonates (less than 1 month of age) have not been established." Please refer to the Zantac Prescribing Information for information on the dosage for pediatric patients.
4According to the Prevacid Prescribing Information “safety and effectiveness of PREVACID have been established in pediatric patients 1 to 17 years of age for short-term treatment of symptomatic GERD and erosive esophagitis, however, PREVACID was not effective in patients with symptomatic GERD 1 month to less than 1 year of age in a multicenter, double-blind, placebo controlled study.” Note: Short-term treatment for pediatric use appears to refer to a period of up to 12 weeks according to the product information.
Please refer to the Prevacid Prescribing Information for more information on the dosage for pediatric patients.
5Tsou - Study was done on "infants with normal renal function during prolonged aluminum-containing antacid use."
Overall, no one can guarantee the medication is safe for your baby and you may be advised by your doctor to give your baby medicine that is not FDA approved.
(To Top)
9. How do I know if my baby has an allergy?
Please refer to the "Introducing Baby Food" article.
Some signs are:
- Spitting up1
- Diarrhea1
- Constipation1
- Blood in the stool1
- Irritability1
- Skin rashes1,2or diaper rash2
- Swelling of face or tongue2
- Congestion such as a stuffy or runny nose lasting more than two weeks2
- Wheezing or rattling in the chest2
- Vomiting2
1Greene,
Feeding 171
2Sears,
Happy Baby 167
Even if your baby is not allergic to the food, your baby could become constipated when you introduce the food as a lot of the first foods can be constipating. If after changing the foods and your baby is still constipated or has very loose stools, "consider the possibility that your baby has a cow's milk protein allergy. It more commonly causes loose stools, but it is also often a cause of constipation" (Greene, Feeding 159). Some babies may experience a food intolerance which is not considered an allergy. According to Sears, symptoms of a food intolerance may be:
- Diarrhea (runny or mucous stools)
- Night waking or fussiness
- Upset stomach, vomiting, gas pains (Happy Baby 167)
(To Top)
10. What may cause an allergic reaction?
Please refer to the "Introducing Baby Food" article.
According to Sears, the foods that account for the 90% of food allergies in children are:
- Cow's milk products
- Egg white
- Fish
- Peanuts
- Shellfish
- Soy
- Tree Nuts (almonds, cashews, and walnuts)
- Wheat (Happy Baby 167 - 168)
A lot of sources recommend waiting until over a year to start the allergy prone foods. Food "such as cheese, yogurt, baby cereals, teething biscuits, breads, egg yolk, mild fish like wild salmon or cod, and tofu" can be started around nine months (Happy Baby 168).
(To Top)
11. What are good medical resources?
Please refer to the "Medical Resources" article.
(To Top)
12. Where can I find a list of all articles?
Please refer below for a summary or to Medical Home page. Or please refer to the the All Articles Home page.
IInfants & Toddlers
All
(To Top)
FAQ's coming soon
Please refer to the Milestones Home page for a list of all milestones articles or the All Articles Home page.
1. How do you pronounce MOMMBY?
You pronounce it just like you say Mommy but with a B.
MOMMY + BABY = MOMMBY
(To Top)
2. When was MOMMBY.com started?
MOMMMBY was born on May 2009 but information was not launched on MOMMBY.com until November 2009.
(To Top)
3.Why Start MOMMBY?
I wanted to offer support, guidance, and encouragement to other parents. To share research and not just present the politically correct answer. Please refer to the"Why" article for more information.
(To Top)
4. Who is the MOMMBY Mom?
Please refer to the "About Me" article. Top 10 random facts about me are...
Please follow
Diary of a Mom for more information.
(To Top)
5. Who inspired MOMMBY.com?
Inspired by Baby. Developed by Mommy.™ Please refer to "Meet My Family" article for more information. Please also refer to the "My Family" articles for more information. Please follow Diary of an Infant and Diary of a 3 Year Old.
(To Top)
6. Did MOMMBY Dad rappel the Washington Monument?
Yes, the MOMMBY Dad was one of the engineers that spent a week rappelling the Washington Monument! Please refer to the "Washington Monument" article for more information. Please also follow Diary of a Dad.
(To Top)
1. How can you promote attachment parenting?
Please refer to the
"Attachment Parenting" article.
The three most important things (in my own mother’s words) about taking care of a child are to provide love and security while following your mommy (or daddy) instinct. I admit as much as I love my baby more than anything being a parent is not an easy job which is why it is nice to have something like the list of things you love about being a parent to reflect on. I encourage you to write your own thoughts down which you may or may not pass on to your child as she grows older. Some other ways to promote attachment are to try “Breastfeeding” or “Baby Wearing.” “Bottle Feeding” can also promote attachment. The attachment comes from being with your baby, listening to your baby, and interacting with your baby. Remember that your baby cries as a way to communicate with you.
(To Top)
2. What are the benefits of baby wearing?
Please refer to the "About Baby Wearing" article.
It supports the E.A.S.Y. schedule, it may reduce crying/colic, may help babies with reflux, promotes bonding, may even help with mental development, allows caregiver to continue with daily activities, and may even allow some "quiet" time with spouse.
(To Top)
3. What are some baby wearing products?
Please refer to the "Baby Wearing Products" article.
There are various products to buy if you want to wear your baby. You can choose a sling or a carrier. We tried everything from the BabyBjorn carrier to the Ergobaby carrier to the Moby Wrap. Overall, the BabyBjorn was still my favorite simply because of the ease of use. The Moby Wrap was really nice for the first few weeks but I just never got the hang of all of the wrapping and so I preferred the easy in easy out style of the BabyBjorn. Ultimately, you have to decide what works best for your family.
(To Top)
4. My baby cries all of the time. Is It colic?
Please refer to the "Crying Baby...Is It Colic" article.
Remember that all babies cry. “The average 6-week-old fusses or cries more than an hour a day. A full 25% cry more than two hours" (CDHNF). So how do you know if your baby is crying the normal amount of time or if your baby is "colicky" or a "hurting baby?" In general:
- " 20 percent of babies suffer from some form of colic"
- Of the 20%, "10 percent are considered severe cases” (Hogg 263).
One way to decide if your baby is a true "colic" or "hurting baby" is to follow the "rule of three"
- last at least three hours a day, occur three days per week, and continue for at least three weeks
- begin within the first three weeks of life
- seldom last longer than three months
- occur in an otherwise healthy, thriving baby (Sears 384)
As described by Sears, some babies may be colicky only in the evening and unfortunately others may be colicky all day. For the evening-only colicky babies, they are usually very happy during the day and people would never know that they are considered colicky at night and these babies tend to sleep well at night. The good news with the evening only colicky babies, generally, “there is rarely an underlying medical cause...” (Sears 384). Based on my mommy instinct, I would think for some of these babies they are simply over exhausted from the day and are having trouble settling down for the night. My son was not colicky but he definitely would have more "fussy" periods at night when he was tired.
On the other hand, the all-day colic baby “is rarely happy” and "[h]e spends most of the day fussing, squirming, or screaming.” In addition, these all day colic babies are usually restless sleepers. This is where the Sears state this baby deserves the "hurting baby" title (Sears 384). My heart goes out to both the babies and the caregivers for these babies.
(To Top)
5. How can I understand my baby's cries?
Please refer to the "Different Meanings" article.
According to Priscilla Dunstan you can understand a baby’s cry. She said the cries can be divided into five different types:
- NEH – Hunger (due to sucking reflex)
- OWH – Sleepy (like baby is yawning)
- HEH – Discomfort (diaper needs changed or hot/ cold)
- EAIR – Lower gas (may pull up legs as well)
- EH – Baby needs to burp
She said that these sounds are "actually sound reflexes" that will generally turn off after the first 3 months unless the cries are appropriately responded to. The baby may continue to make the sounds if it gets the response it wanted. The other important thing to note according to Dunstan is these sounds are more the "pre-cry" the beginning sounds the baby makes. If the baby is not attended to, then this "pre-cry" will turn into a full cry and the sounds will be harder to distinguish.
I believed this woman but I wasn’t sure I would be able to distinguish the difference with my baby. Although, Erik and I were pretty sure that most of the time we could tell the difference. The NEH and the OWH were probably the most distinguishable.
(To Top)
6. Does parenting get easier?
Please refer to the "Does It Get Easier" article.
Unfortunately, I do not think parenting should get easier, that is why in Oprah’s words, “Being a mother is the hardest job on earth.” With that said, I also think parenting can be the most rewarding task anyone can do and I’m grateful every day for my babies. I couldn’t imagine life without them. Please refer to the "I Love" article for just a few things I love. That does not mean that every minute of every day is easy. Each stage of development will bring something special to cherish, first smile, first time sitting, first time standing, first time walking, first time eating, first time having a real conversation, first time playing ball, first friend, first day of school, first girlfriend, first job, the list will never end.
(To Top)
7. How do I give my child the greatest gift?
Please refer to the "Greatest Gift - Gift of Health" article.
I believe the greatest gift you can give your family is the gift of health! I believe one way to give the gift of health is to truly know what you are feeding your family, look at the ingredients in products you are buying and try to buy organic to avoid pesticides, artificial hormones, antibiotics, genetically modified organisms, artificial colors and preservatives, and added nitrates.
(To Top)
8. What are some nighttime parenting tips?
Please refer to the "Nighttime Parenting" and "Tips: To Help Sleep" articles.
Some nighttime parenting tips we did for our babies were to create a secure environment, try different soothing methods and focus on "sensible sleep" rather than the cry it out approach.
Most of the research I read discussed the importance of a daily and nighttime routine to help the baby sleep well at night. According to Sears, if your baby has a consistent nap routine then she may be "more likely to sleep longer stretches at night” ("31 Ways"). In addition to a daily routine, a nightly routine really worked well for us. Secrets of Baby Whisperer by Tracy Hogg , Healthy Sleep Habits, Happy Children by Marc Weissbluth, M.D., The Baby Book by William Sears, M.D., and Martha Sears, R.N., or Dr. Spock’s Baby and Child Care by Benjamin Spock, M.D. all were books that promoted some sort of bedtime routine.
Making sure your baby is well fed generally will help her sleep better at night. A lot of research promotes putting the baby to sleep before she gets overtired. In our experience our baby always slept best when he was well rested. You will want to make sure your baby is dressed appropriately, ideally in 100% cotton pajamas, and warm enough. If it is in the colder months you may want to try a sleep sack or dress in two sets of pajamas but you also do not want your baby to be too warm.
Determining the best sound to help calm your baby also helps get her ready for sleep. Whether it is you talking or singing to your baby, the sound of the vacuum cleaner, static on the radio, heartbeat or womb sounds, or a traditional lullaby.
(To Top)
9. Should I follow a schedule?
Please refer to the "Schedule Versus Demand" article.
Although I love schedules, surprisingly, my daily schedule is not very strict since my schedule evolves each day to best meet both my and my baby’s needs. Most books promote a schedule for babies since the routine helps calm babies because it helps them know what to expect.
Even if you aren’t a “schedule” type person in a way a baby forces you to get into some sort of schedule whether you like it or not. Sleep, eat, activity, bathroom, sleep, eat, bathroom, activity, the order may switch around but basically they eat, sleep, and do some sort of activity which generally is simply going to the bathroom. Obviously there are a lot of wonderful moments that occur in those early weeks but in addition to those moments basically for the first month or so the baby eats, sleeps, and goes to the bathroom.
Before I had my son I read about the E.A.S.Y. (Eat, Activity, Sleep, You) schedule describe in Secrets of the Baby Whisperer by Tracy Hogg. In general the E.A.S.Y schedule is somewhere in the middle between “On Demand” and a strict “Schedule” which is why it appealed to me
As discussed in HEALTHY SLEEP HABITS, HAPPY CHILD BY Marc, Weissbluth, M.D. “bedtime routines help all children calm down before falling asleep…”(75).
No matter whether you follow a schedule or not, I would recommend at least occasionally documenting your normal day. Refer to this template to document a schedule for a baby 0-6 months and this template for a baby 6+ months.
(To Top)
10. Why and how do I document my baby's schedule?
Please refer to the "Document Daily Schedule" and the "Template" articles.
No matter whether you follow a schedule or not, I would recommend at least occasionally documenting your normal day. I think it is very important to document for several reasons: it helps establish the baby’s routine: when does the baby tend to sleep, eat, and go to the bathroom. This will enable you to determine what is “normal” for your baby and thus if something changes you can analyze to find out what changed and or if something is wrong with your baby.
Refer to this template to document a schedule for a baby 0-6 months and this template for a baby 6+ months.
(To Top)
11. What are some soothing techniques?
Please refer to the "Soothing Techniques" article.
It is inevitable, all babies will cry at some point. The faster you are able to meet your baby's needs usually the less your baby will cry. It may help to learn the different meanings of a baby's cry. You may want to combine parent soothing methods along with self soothing methods. Some baby's like to use a pacifier. YOu may want to try different holds or use motion such as rocking, baby wearing, baby swing, walking, riding in a stroller, or going for a car ride.
(To Top)
12. What are good parenting resources?
Please refer to the "Parenting Resources" article.
(To Top)
13. Where can I find a list of all articles?
Please refer below for a summary or to the Parenting Home page for a list of all parenting articles or the All Articles Home page.
Infants & Toddlers
All
(To Top)
1. About Peek-a-Bye-Baby™ Cover
Please refer to the MOMMBY Store page.
The patent pending Peek-a-Bye-Baby™ cover functions as a nursing cover and a burp cloth. It's the nursing cover for baby to see mother and burp cloth that won't fall off.™
The MOMMBY Peek-a-Bye-Baby™ cover was inspired by my first baby who unfortunately suffered from reflux. I was constantly changing my shirt because the burp cloths did not provide adequate coverage. In addition, the burp cloths were always falling off my shoulder.
My second baby provided the inspiration to re-design the cover to better accommodate nursing. I enjoyed using the cover for privacy while having the ability to peek at my baby since she was not hidden under a large nursing cover.
I hope the MOMMBY Peek-a-Bye-Baby™ cover makes feeding, burping, and caring for your baby easier. I wish you and your family the best.
DO NOT USE COVER AS BABY WEARING DEVICE.
COVER WILL NOT SUPPORT BABY!
Please refer to the "About" article for more information.
(To Top)
2. Shipping Information
Products will only be shipped to a U.S. address. We currently offer US Postal Priority Shipping. Currently a $5 shipping charge is applied to any order less than $40. Rates may be adjusted to reflect the total amount of the order and where the package is being shipped. You will receive an email informing you the package has been shipped.
Once we receive an order it is processed and shipped as soon as possible. All orders are processed on Monday through Friday from Virginia State. Please allow 7-10 business days to receive your order. We will notify you if there is going to be a delay with your order. If you need the product quickly, please email us at sales@mommby.com.
(To Top)
3. Sales Tax
Any order shipped to a Virginia State Address is subject to Virginia Sales tax of 5%.
(To Top)
4. Returns
If you are not 100% satisfied with the MOMMBY™ products purchased through the MOMMMBY Store they can be returned for a full refund up to 30 days of purchase as long as they are in new, unworn/unwashed, and in resalable condition. Item will be inspected upon receipt and if it does not meet our return qualifications it will be sent back at the customer's cost. The refund will not include shipping charges previously paid or shipping paid to send the product back to us. For products purchased through the MOMMBY Amazon Store please refer to Amazon for return policies for Amazon products. Please refer to the "Returns" article for more information.
(To Top)
1. Favorite toys for an infant?
Please refer to the
"Infant Play" article.
Some of my favorite toys for an infant are baby wearing products, music and books, play mat, bouncer, activity jumper or activity center, music table and push toys, household items, soft blocks, ring stack, and educational DVD's like Tiny Love MagIQ and the Baby Einstein videos. Please refer to the MOMMBY Amazon Store, specifically the Toys - Infants and DVD's - Infants for some products.
(To Top)
2. Favorite toddler toys?
For toddlers, I feel it is a big transitional phase where they will be transitioning from the infant toys to the preschooler toys. Some of our favorite toys are activity centers, blocks, stackers, magnetic letter fridge set, nesting toys, shape sorters, and push toys.
Please refer to the MOMMBY Amazon Store, specifically the Toys - Toddlers and DVD's - Toddlers for some products.
(To Top)
3. Favorite preschooler toys?
Please refer to the "Preschooler Play" article.
It is fun to watch your preschooler mature and play independently. I love watching the pretend/imaginary play. My preschooler loves all different types of play from outdoor physical play riding on his scooter or bike to drawing to doing puzzles and board games.
Please refer to the MOMMBY Amazon Store, specifically the Toys - Toddlers and DVD's - Toddlers for some products.
(To Top)
4. What are some craft ideas?
Please refer to the
"Craft Ideas" article.
When my son just turned two we did a Mommy and Me preschool class together and he wasn't into the crafts at first. Then as he got older and attended preschool on his own he started to enjoy the various craft activities. Anything involving tracing their hands are fun. At thanksgiving, we made turkeys. He colored his turkey by himself. We try to do a special craft each holiday season.
5. Where can I find a list of all articles?
Please refer to the Play Time Home page for a list of all play time articles or the All Articles Home page.
(To Top)
1. Help with Baby Names?
Please refer to the "Baby Names" article.
Picking your baby name is a very personal decision which is why we decided to keep the name to ourselves so we did not receive feedback from others that would cause us to change the name. We knew we liked the names and felt the names would be perfect for our kids. If you need some resources to help you come up with names, you may want to get something like 100,000+ Baby Names by Bruce Lansky out of the library.
(To Top)
2. What are things to help pregnant mommy?
Please refer to the "For Mommy" article.
My favorite thing was the pregnancy body pillow. Some other things you may want/need are belly cream, maternity band, and maternity clothes.
(To Top)
3. How do I prepare for the birth?
Please refer to the "Preparing for Birth" article.
You may be interested to read pregnancy books. Some people love reading the books and others find it overwhelming or unnecessary. If you only have time or want to read one book you may be interested to read a book about how to help your baby sleep at night like Secrets of the Baby Whisperer: How to Calm, Connect, and Communicate with Your Baby by Tracy Hogg with Melinda Blau. I enjoyed reading this book as it went along with my parenting philosophy to truly listen to my baby. Please refer to the "Secrets" article for more information on this book.
You will want to pre-register for your hospital. You may want to take a birthing class or at least rent an informational birthing video from your local library, pick out your baby's name, decide if you want to do breastfeeding, bottle feeding, or both, buy some baby supplies (refer to the "Baby Registry List" article, pick our your baby's doctor, install the baby car seat, and pack your bag for the hospital.
(To Top)
4. What are the top baby registry items?
Please refer to the "Baby Registry" article.
My top ten must have items most of which can be found at The MOMMBY Amazon Store - Featured Items.
- MOMMBY™ Peek-a-Bye-Baby™ Cover
- Summer Infant Sleek and Secure Handheld Color Monitor
- BabyBjorn Carrier
- Boppy Pillow
- Miracle Blanket
- Dr. Brown's Bottles or Tommee Tippee Bottles
- Medela Pump in Style Advanced Breast Pump
- Baby Einstein Play Mat
- Fisher Price Bouncer Chair
- The Baby Book: Everything You Need to Know About Your Baby
(To Top)
5. What should I take to the hospital?
Please refer to the "Take to Hospital" article.
- BEFORE BIRTH
- Driver's License
- Insurance Card
- Hospital Paperwork
- Birth Plan (If You Have One)
- Things to Help Relax
- Clear Liquid Foods
- FOR YOU
- Nightgown with Buttons In Front
- Bras
- Old Underwear (Several Pairs)
- Bra Pads & Panty Pads
- Going Home Outfit
- Beauty Products
- Hair Products
- Toothbrush & Tooth Paste
- Glasses & Contacts
- IF BREASTFEEDING
- Nursing Bra
- Pump Machine (Rent from Hospital)
- Breast Cream
- Nipple Shields
- Breastfeeding Cover or Boppy Pillow
- IF BOTTLE FEEDING
- CAMERA & OTHER ITEMS
- Camera and/or Video Camera
- Batteries, Charger, Memory Card
- Snacks
- Cell Phone & Charger
- List of Friends to Call/ Email
- Insurance Information
- Notebook or Journal
- FOR SPOUSE
- Change of Clothes
- Socks, Underwear
- Pajamas
- Wallet with Money
- Bathing Suit
- FOR SIBLING
- Clothes
- Snacks
- Toys
- Gift from Baby
- FOR BABY
- Installed Infant Car Seat
- Going Home Outfit
- Swaddling Blankets
- Diapers - Hospital Will Provide
(To Top)
6. What are good resources?
Please refer to the "Pregnancy & Delivery Resources" article.
(To Top)
7. Where can I find a list of all articles?
Please refer to the Pregnancy & Delivery Home page for a list of all pregnancy & delivery articles or the All Articles Home page.
(To Top)
1. What are the benefits of baby wearing?
Please refer to the
"About Baby Wearing" article.
It supports the E.A.S.Y. schedule, it may reduce crying/colic, may help babies with reflux, promotes bonding, may even help with mental development, allows caregiver to continue with daily activities, and may even allow some "quiet" time with spouse.
(To Top)
2. What are some baby wearing products?
Please refer to the "Baby Wearing Products" article.
There are various products to buy if you want to wear your baby. You can choose a sling or a carrier. We tried everything from the BabyBjorn carrier to the Ergobaby carrier to the Moby Wrap. Overall, the BabyBjorn was still my favorite simply because of the ease of use. The Moby Wrap was really nice for the first few weeks but I just never got the hang of all of the wrapping and so I preferred the easy in easy out style of the BabyBjorn. Ultimately, you have to decide what works best for your family.
(To Top)
3. Any car seat recommendations?
Please refer to the "Car Seat" article.
You will want to make sure your car seat is successfully installed. To see if your car seat is installed properly and to find a certified passenger safety technician in your area, visit www.SeatCheck.org or contact Child Safety Seat Inspection Station Locator. You can call 866-SEAT-CHECK (866-732-8243) or 888-327-4236 or you could also call your local police or fire departments (NON-EMERGENCY) lines to find out if they offer car seat checks.
To select your baby's car seat you'll need to determine if you want to start with an infant carrier or a convertible car seat.
(To Top)
4. What about child care?
Please refer to the "Child Care" article.
There are many different types of care to find for your child. Whether it is a Nanny, Daycare, or care at someone else's home only you will know the right place for your child. You may want the individual attention provided by a Nanny or you may prefer the structured setting of a daycare. You may like the "homey" feel of the care at someone's house. The only way you'll determine the right place for your child is to investigate your options. Make sure you ask various questions to make sure you are comfortable with the care your baby will receive.
If you just need a short "break" you may want to look into a Mother's Day Out program. Various churches usually offer at least one morning varying between 2 - 4 hours for a baby usually starting around 1 year old where the Mother can have a "morning out" to herself. Once the child is closer to 2 1/2 to 3 years old there are a lot more preschool options available. My favorite thing was joining a gym with daycare. I found joining a gym with daycare was the most cost effective outside care option if you simply want a few hours to do something for yourself. (You generally need to stay onsite when using the gym care facilities.)
(To Top)
5. My baby cries all of the time?
Please refer to the "Crying Baby...Is It Colic" article.
Remember that all babies cry. “The average 6-week-old fusses or cries more than an hour a day. A full 25% cry more than two hours" (CDHNF). So how do you know if your baby is crying the normal amount of time or if your baby is "colicky" or a "hurting baby?" In general:
- " 20 percent of babies suffer from some form of colic"
- Of the 20%, "10 percent are considered severe cases” (Hogg 263).
One way to decide if your baby is a true "colic" or "hurting baby" is to follow the "rule of three"
- last at least three hours a day, occur three days per week, and continue for at least three weeks
- begin within the first three weeks of life
- seldom last longer than three months
- occur in an otherwise healthy, thriving baby (Sears 384)
As described by Sears, some babies may be colicky only in the evening and unfortunately others may be colicky all day. For the evening-only colicky babies, they are usually very happy during the day and people would never know that they are considered colicky at night and these babies tend to sleep well at night. The good news with the evening only colicky babies, generally, “there is rarely an underlying medical cause...” (Sears 384). Based on my mommy instinct, I would think for some of these babies they are simply over exhausted from the day and are having trouble settling down for the night. My son was not colicky but he definitely would have more "fussy" periods at night when he was tired.
On the other hand, the all-day colic baby “is rarely happy” and "[h]e spends most of the day fussing, squirming, or screaming.” In addition, these all day colic babies are usually restless sleepers. This is where the Sears state this baby deserves the "hurting baby" title (Sears 384). My heart goes out to both the babies and the caregivers for these babies.
(To Top)
6. Can I understand my baby's cries?
Please refer to the "Different Meanings" article.
According to Priscilla Dunstan you can understand a baby’s cry. She said the cries can be divided into five different types:
- NEH – Hunger (due to sucking reflex)
- OWH – Sleepy (like baby is yawning)
- HEH – Discomfort (diaper needs changed or hot/ cold)
- EAIR – Lower gas (may pull up legs as well)
- EH – Baby needs to burp
She said that these sounds are "actually sound reflexes" that will generally turn off after the first 3 months unless the cries are appropriately responded to. The baby may continue to make the sounds if it gets the response it wanted. The other important thing to note according to Dunstan is these sounds are more the "pre-cry" the beginning sounds the baby makes. If the baby is not attended to, then this "pre-cry" will turn into a full cry and the sounds will be harder to distinguish.
I believed this woman but I wasn’t sure I would be able to distinguish the difference with my baby. Although, Erik and I were pretty sure that most of the time we could tell the difference. The NEH and the OWH were probably the most distinguishable.
(To Top)
7. What if my baby spits up all of the time?
Please refer to the "About Reflux" article for more information.
All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
(To Top)
8. What is infant reflux?
Please refer to the "About Reflux" article for more information.
According to Children’s Digestive Health and Nutrition Foundation, (CDHNF) “Gastroesophageal Reflux occurs when an infant’s muscular sphincter-- where the esophagus enters the stomach-- allows acidic, gastric (stomach) fluids to reflux, or flow backwards up into the esophagus and sometimes reach as high as the mouth or nose” (CDHNF, "Coping"). All babies initially have some form of reflux as it "is a normal part of maturation and development that gets better during the first year of life" (CDHNF, "Coping").
Most babies will spit up and they won't be bothered by it but some babies have reflux that causes pain that adults would refer to as heartburn. In addition, if “reflux causes troublesome symptoms or complications such as failure to gain weight, bleeding, respiratory problems or esophagitis" it is referred to as gastroesphageal reflux disease (GERD) (CDHNF, "Pediatric").
The following are some facts about reflux and GERD:
- "The majority of infants do not experience problems from reflux"1
- "More than 50% of babies spit up regularly in the first months of life"1
- "Reflux usually peaks at 4 months and stops by 12 – 18 months"1
- "Spitting up crosses the line into GERD when the infant begins to show symptoms including refusal to feed, poor weight gain, breathing problems and others."1
- "[R]eflux (GER) and cow milk allergy (CMA) occur frequently in infants younger than 1 year....up to half of cases of GER in infants...may be an association with CMA....[and] also CMA induced."3
- Reflux is "[o]ne of the most common hidden medical causes of nightwaking (and colicky behavior)...."4
- "In many cases GERD in kids can be managed with lifestyle changes, and without medication"1
- "GERD often runs in families"1
- "Kids with GERD may have frequent complaints of abdominal pain or a tummy ache"1
- "Children and teens with asthma are more likely to have GERD"2
1CDHNF, "Quick Facts about Reflux and GERD"
2CDHNF, "Pediatric"
3Salvatore
4Sears, "31 Ways"
(To Top)
9. What can you do for infant reflux?
Please refer to the "About Reflux" article for more information.
Your pediatrician may recommend a trial of medication that decreases acid in your baby's stomach or refer you to a GI specialist. Our son was put on medication when he was six months old and was on it until about 2 1/2 when he finally seemed to grow out of his reflux. Before my son turned 2 1/2 we tried taking him off the medication several times but he usually would stop eating well and become "needy" when he was usually very independent. When my son was around 2 years old at a visit to the GI specialist she increased his medication as she said the most important thing is to make sure his esophagus is not damaged by the acid. Please refer to the "Medication" article for more information.
If the GERD is extreme then surgery may be recommended. There are also "lifestyle adjustments" that can help a baby:
- "Avoid overfeeding"1
- "Don't feed the baby again after he or she spits up (wait until the next feeding time)"1
- "Check with your doctor to see if you are using appropriately sized bottles or nursing the appropriate amount of time"1
- Our baby drank best with the Dr. Brown's bottles."
- Feed half as much twice as often."2
- Starting at 4 months, our baby would only drink a few ounces at a sitting and so we had to do frequent feedings to help ensure he drank enough for the day.
- "Feeding frequently stimulates more saliva production...[and] [s]alivia contains a healing substance...which helps repair the damaged tissues in the esophagus. It also neutralizes stomach acid and lubricates the irritated lining of the esophagus."2
- If possible, breastfeed your baby
- "[E]asy-in, easy-out" since it empties from the stomach faster and usually produces "softer and easier-to-pass stools"2
- "Breast milk is more intestine friendly than formula."2
- I was able to breastfeed my baby until around 6 months and had I known breast milk would have helped his reflux I would have tried to breastfeed longer. Unfortunately, my son's reflux contributed to weaning from breastfeeding early since around 4 months he didn't want to breastfeed (or bottle feed) and so I started doing more bottles so I could track what he was drinking for the day.
- "If your baby is formula-fed, thicken the formula with a small amount of rice cereal"1
- We switched to oatmeal cereal as it was not as constipating as rice cereal was for our baby.
- Try different formulas, our baby digested Nestle Good Start better than other formulas since it was 100% whey rather than the whey/casein mix of most formulas.
- You may want to try a Hypoallergenic formula to see if your baby has a cow milk allergy.
- Make sure you burp baby well as excess "air aggravates reflux"2
- For awhile, we were hesitant with burping our baby since he got so upset when we burped him but really that was the best thing for him. We found that if we gave him his pacifier when we were burping him that it helped.
- Try other bottles to help minimize air intake or make sure baby is properly latched on for breastfeeding.
- "Keep the baby upright for at least 30 minutes after a feeding."1
- Wear your baby to help keep her upright; I think this helped my baby for the first few months.
- Try to not "jostle or vigorously play with baby after feedings"2 I still try to remind our son's Daddy to try to not play too much right after our son (now almost two years old) eats but that is hard for both him and my son to follow.
- Discuss with your doctor about positioning the baby at night to sleep. It is recommended to put the baby to sleep on her back to help avoid SIDS (Sudden Infant Death Syndrome) but if your baby is suffering from reflux you may want to discuss other sleep positions.
- We elevated our baby's mattress. You can also buy sleep positioners some of which are elevated for the baby. We should have bought one of these.
- "Try not to let your baby spend too much time in a car seat (The baby's position in the car seat can promote reflux)"1
- "Avoid tight diapers and elastic waistbands"1
- Develop parenting style to promote attachment parenting to help decrease crying, "since crying puts pressure on the stomach which worsens the reflux"2
- Pacifier use may help since "sucking stimulates saliva production"2 unless the baby sucks too hard and swallows air then the air can make the reflux worse.
- My son always loved his pacifier and I was happy to let him use something that made him feel better.
- My son is almost two and I still let him have his pacifier for nap and bedtime. I plan to wean in the next year although since he is still suffering from reflux I'm reluctant to wean him. My son's pediatric dentist said we should try to wean him before he turns four. I don't think we should have a problem with that.
- Help baby avoid constipation since "increasing abdominal pressure...can aggravate reflux"2
- Unfortunately, my son had constipation for most of his first year which probably didn't help his reflux.
- Oatmeal cereal was less constipating than rice cereal
- When starting baby food, make sure you avoid or limit the constipating foods like bananas, carrots, and applesauce.
- The "Constipation" article is coming soon
1CDHNF, "GERD in Infants: Treatment and Management"
2Sears, The Baby Book 392 - 397
(To Top)
10. What are some soothing techniques?
Please refer to the "Soothing Techniques" article.
It is inevitable, all babies will cry at some point. The faster you are able to meet your baby's needs usually the less your baby will cry. It may help to learn the different meanings of a baby's cry. You may want to combine parent soothing methods along with self soothing methods. Some baby's like to use a pacifier. YOu may want to try different holds or use motion such as rocking, baby wearing, baby swing, walking, riding in a stroller, or going for a car ride.
(To Top)
11. How do I pick a stroller?
Please refer to the "Stroller" article.
There are a lot of strollers to choose from: lightweight strollers, travel system strollers, full-size strollers, double & triple strollers, and jogging strollers. You'll want to compare versatility, size, weight, and price when determining the best stroller for your family.
It is generally recommended to carry the baby in a stroller that "reclines fully (to an almost flat position) until your baby is around 6 months old" (BabyCenter). A lot of people use a stroller that accommodates the infant carrier (infant car seat). The infant carrier can be put into a stroller frame or in one of the travel systems that is built to accommodate an infant carrier. Not all strollers are able to use an infant carrier thus, if you want to be able to properly use the infant carrier with a stroller make sure it is compatible to do this.
Strollers come in many different sizes and weights. For us, we tried to find the smallest (or at least the stroller that could get the most compact) and also the lightest. That is why we went with the Graco SnugRide travel frame, and then moved onto the Combi Cosmo EX Stroller and then moved onto the Especially for Kids Umbrella Stroller (probably my favorite for short trips as not very padded).
(To Top)
12. When can my baby wear sunblock?
Please refer to the "Sunblock" article.
Summer is a wonderful time for children but it is also important to make sure you protect your kid's skin. According to the American Academy of Pediatrics (AAP), some sunblock can be used for babies less than 6 months old but try to limit the use to "small areas of the body, such as the face and the backs of the hands, if protective clothing and shade are not available." Once the baby is older than 6 months then "[a]pply to all areas of the body, but be careful around the eyes" (AAP). The reason to avoid the use of sunblock for babies less than 6 months old is "[b]ecause of the uncertain absorption of sunscreen through the skin of tiny babies...[u]se it sparingly..." (Sears 735).
The best sunblock is to try to keep babies in the shade, use hats, and protective clothing. It was easy for my sun as I loved using the bathing suit tops that had the UV protection. For my baby girl her bathing suit doesn't cover much of her skin so I had to use extra precautions.
Try to find a sunscreen with the following elements:
- "Broad Spectrum" - both UVB and UVA
- SPF of at least 15. (Higher SPF more UVB protection)
- UVA Star Rating: 1 star - low; 2 stars - medium; 3 stars - high; 4 stars - highest protection in over-the counter sunscreen product
- For extra sensitive areas (nose, cheeks, tops of ears, shoulders) use one with zinc oxide or titanium dioxide which will stay visible on skin even after you rub them in
- Use PABA-free since some babies are sensitive to PABA
- Use waterproof sunblock
- Apply 30 minutes before going outside
- Use even on cloudy days; remember sun reflects off of water and sand
- Reapply every 2 hours especially if swimming or sweating
(To Top)
13. What are good routine care resources?
Please refer to the "Routine Care Resources" article.
(To Top)
14. Where can I find a list of all articles?
Please refer to the Routine Care Home page for a list of all routine care articles or the All Articles Home page.
Infants & Toddlers
All
(To Top)
1. Do babies have to sleep on their back?
Please refer to the
"About Baby Sleep" article.
“The American Academy of Pediatrics has recommended since 1992 that infants be placed to sleep on their backs to reduce the risk of sudden infant death syndrome (SIDS).”
(To Top)
2. Will my baby sleep through the night?
Please refer to the "About Baby Sleep" and the "Nighttime Weaning" articles.
According to the Disney article, most babies can sleep without waking to eat according to the following schedule:
Age |
Time Before Waking to Eat |
| 3 weeks - 4 months |
Range (2 - 6 hours) |
| 4 months |
6 hours |
| 5 months |
9 hours |
| 6 months |
12 hours |
Remember, that the above schedule is the "norm" for most babies. Each baby is an individual and if "your child was a preemie or has acid reflux, he'll likely need to eat more often..." (Disney). We were very fortunate with my son and daughter in that overall they slept fairly well. I think it was a combination of our nighttime parenting, their temperaments, whether they were teething or not, and how much they were able to eat during the day. My son and daughter slept at night according to the following schedule:
Baby's Age |
My Son's Time Before Waking to Eat |
My Daughter's Time Before Waking to Eat |
Total Sleep Time* |
| Newborn |
4 hours |
4 hours |
14 - 18 hours |
| 1 months |
4 - 6 hours |
4 - 6 hours |
14 - 18 hours |
| 2 months |
6 - 8 hours |
6 - 8 hours |
14 - 18 hours |
| 3 months |
8 - 10 hours |
6 - 8 hours |
14 - 16 hours |
| 4 - 6 months |
8 - 12 hours |
6 - 8 hours |
14 - 16 hours |
| 6 - 7 1/2 months |
4 - 6 hours |
10-12 hours |
12 - 14 hours |
| 7 1/2 -10 1/2 months |
4 - 6 hours |
5-12 hours |
12 - 14 hours |
| 10 1/2 - 13 months |
12 hours |
OPEN |
12 - 14 hours |
| 13 - 15 months |
6 - 8 hours |
OPEN |
12 - 14 hours |
| 16+ months |
12 hours |
OPEN |
12 - 14 hours |
*The total sleep time is the time for the entire day including naps according to Sears (357).
(To Top)
3. How much should my baby sleep?
Please refer to the "Sleep Amount" article.
| Age |
Total Sleep (Hours) |
Duration Night Sleep |
Nighttime Wakings |
Naps |
Duration of Naps (Hours) |
Notes |
| 1st week |
16.5 or
14 - 18 |
|
|
|
|
Don’t sleep more than 2 – 4 hours at a time. |
| 0 - 1 Month |
15.5 or
14 - 18 |
|
|
|
|
May only sleep 4 hours before waking. |
| 1 - 2 Months |
15.5 or
14 - 18 |
|
|
M, A, E |
|
May only sleep 4 hours before waking.
(My son slept 4 - 6 then 6 - 8 ) |
| 3 - 4 Months |
15 or
14 - 16 |
10 - 12 |
0, 1, 2 |
M, A, E |
2 - 4 |
By 4 months, usually can sleep 6 hours straight before waking to eat. |
| 5 - 6 Months |
14.25
14 - 16 |
10 - 12 |
0, 1, 2 |
M, A |
2 - 4 |
May still take 3 naps. By 5 months usually can sleep 9 hours, by 6 months usually can sleep 12 hours before waking to eat. |
|
| 7 - 8 Months |
14 or
12 - 14 |
10 - 12 |
0, 1, 2 |
M, A |
2 - 4 |
|
| 9 - 10 Months |
14 or
12 - 14 |
10 - 12 |
|
M, A |
2 - 4 |
|
| 11 - 12 Months |
13.75 or
12 - 14 |
10 - 12 |
|
M, A |
2 - 4 |
May only take one long nap |
| 13 - 24 Months |
12 - 14 |
10 - 12 |
|
A |
2 - 4 |
|
| 2 - 5 Years |
10 - 12 |
10 - 12 |
|
A |
|
May still take a nap. Usually by 3 years old afternoon nap become less common. |
(To Top)
4. Why is my baby waking?
There are many reasons the baby may be waking up. Some medical or physical causes could be Gastroesphageal reflux (“GER”) or acid reflux, allergies, teething, cold, fever, ear infection, too hot or cold, pinworms. Some other causes could be developmental, separation anxiety, emotional, or the baby’s temperament (Sears, Baby 325-329). The article that provides more information on nightwaking is coming soon.
During the 6 month to 10 ½ month period, I think my son’s nightwakings were due to a combination of acid reflux, teething discomfort, wakings to practice milestones, and lack of sufficient food during the day.
(To Top)
5. What are some nighttime parenting tips?
Please refer to the "Nighttime Parenting" and "Tips: To Help Sleep" articles.
Some nighttime parenting tips we did for our babies were to create a secure environment, try different soothing methods and focus on "sensible sleep" rather than the cry it out approach.
Most of the research I read discussed the importance of a daily and nighttime routine to help the baby sleep well at night. According to Sears, if your baby has a consistent nap routine then she may be "more likely to sleep longer stretches at night” ("31 Ways"). In addition to a daily routine, a nightly routine really worked well for us. Secrets of Baby Whisperer by Tracy Hogg , Healthy Sleep Habits, Happy Children by Marc Weissbluth, M.D., The Baby Book by William Sears, M.D., and Martha Sears, R.N., or Dr. Spock’s Baby and Child Care by Benjamin Spock, M.D. all were books that promoted some sort of bedtime routine.
Making sure your baby is well fed generally will help her sleep better at night. A lot of research promotes putting the baby to sleep before she gets overtired. In our experience our baby always slept best when he was well rested. You will want to make sure your baby is dressed appropriately, ideally in 100% cotton pajamas, and warm enough. If it is in the colder months you may want to try a sleep sack or dress in two sets of pajamas but you also do not want your baby to be too warm.
Determining the best sound to help calm your baby also helps get her ready for sleep. Whether it is you talking or singing to your baby, the sound of the vacuum cleaner, static on the radio, heartbeat or womb sounds, or a traditional lullaby.
(To Top)
6. What are good sleep resources?
Please refer to the "Sleep Resources" article.
(To Top)
7. Where can I find a list of all articles?
Please refer to the Sleep Home page for a list of all sleep articles or the All Articles Home page.
Infants & Toddlers
All
(To Top)
- Where can I meet other moms and dads?
- What are good support for parents resources?
- Where can I find a list of all articles?
Where can I meet other moms and dads?
(To Top)
2. What are good support for parents resources?
Please refer to the "Support for Parents Resources" article.
(To Top)
3. Where can I find a list of all articles?
Please refer to the Support for Parents Home page for a list of all Support for Parents articles or the All Articles Home page.
(To Top)
1. What should I take to the swimming pool?
Please refer to the
"Pool Time" article.
You will want to take things like sunblock, swim diapers, swim accessories, and snacks. Remember that according to the American Academy of Pediatrics (AAP), some sunblock can be used for babies less than 6 months old but try to limit the use to "small areas of the body, such as the face and the backs of the hands, if protective clothing and shade are not available." Once the baby is older than 6 months then "[a]pply to all areas of the body, but be careful around the eyes" (AAP). The reason to avoid the use of sunblock for babies less than 6 months old is "[b]ecause of the uncertain absorption of sunscreen through the skin of tiny babies...[u]se it sparingly..." (Sears 735).
(To Top)
2. What type of activities do you do in the Spring? In the Summer?
In the spring we love going on Easter Egg Hunts with the kids. If you live in Northern VA, please check out some of our favorite Spring Festivals.
This summer we are excited about attending all of the wonderful free and discounted cultural events. If you live in Northern VA, please refer to the Free Summer Activities in Northern VA as published on Yahoo.
3. Where can I find a list of all articles?
Please refer to the Travel Home page for a list of all travel articles or the All Articles Home page.
(To Top)
American Academy of Pediatrics (AAP). "Changing Concepts of Sudden Infant Death
Syndrome:
Implications for Infant Sleeping Environment and Sleep Position.
" Pediatrics: Official Journal of the
American Academy of Pediatrics. 105 (2000): 650-
656.
18 Dec. 2009
<http://pediatrics.aappublications.org/cgi/content/abstract/105/3/650>.
---. Sun Safety: What's the best way to protect my child in the sun?" healthychildren. 1 June 2011 <http://www.healthychildren.org>.
American Academy of Family Physicians (“AAFP”). “Prevention of Iron Deficiency in Infants and
Toddlers. " American Family Physician. 8 Dec. 2009.
<http://www.aafp.org/afp/20021001/1217.html>.
BabyCenter. "Buying Guide: Strollers." BabyCenter. 18 Jan 2010
<http://www.babycenter.com/0_buying-guide-strollers_10310517.bc>.
---. "Sample Baby Schedules for 1- and 2-Month-Olds." BabyCenter. 15 Dec. 2009
<http://www.babycenter.com/0_sample-baby-schedules-for-1-and-2-month>.
---. "Sample Baby Schedules for 3- and 4-Month-Olds." BabyCenter. 15 Dec. 2009
<http://www.babycenter.com/0_sample-baby-schedules-for-3-and-4-month>.
---. "Sample Baby Schedules for 5- and 6-Month-Olds." BabyCenter. 15 Dec. 2009
<http://www.babycenter.com/0_sample-baby-schedules-for-5-and-6-month>.
---. "Sample Baby Schedules for 7- and 8-Month-Olds." BabyCenter. 15 Dec. 2009
<http://www.babycenter.com/0_sample-baby-schedules-for-7-and-8-month>.
---. "Sample Baby Schedules for 9- and 10-Month-Olds." BabyCenter. 15 Dec. 2009
<http://www.babycenter.com/0_sample-baby-schedules-for-9-and-10-month>
---. "Sample Baby Schedules for 11- and 12-Month-Olds." BabyCenter. 15 Dec. 2009
<http://www.babycenter.com/0_sample-baby-schedules-for-11-and-12-month>
Children's Digestive Health and Nutrition Foundation (CDHNF). "GERD in Infants: Pediatric
GERD in
Infants." 1 April 2010 <http://cdhnf.org/wmspage.cfm?parm1=43>.
---. "Parent's Checklist for REFLUX in Infants 0-12 months old." 29 March 2010.
<http://cdhnf.org/user-assets/documents/pdf/GERD_Checklist.pdf>.
---. "Pediatric Reflux and GERD." 29 March 2010 <http://cdhnf.org/wmspage.cfm?parm1=42>.
Children's Digestive Health and Nutrition Foundation (CDHNF), et al. "Coping When Your
Baby Has Reflux or GERD: You Are Not Alone." CDHNF. 23 March 2010
<http://cdhnf.org/user-assets/documents/pdf/Coping_Reflux_GERD_Guide.pdf>
Disney. "Parentpedia: Nighttime Feeding. " Disney Family Parenting. 8 Dec. 2009.
<http://family.go.com/parentpedia/baby/sleep/baby-nighttime-feeding>.
Eiger, Marvin S. M.D. and Sally Wendkos Olds. The Complete Book of Breastfeeding. New
York: Workman, 1999.
Gerber. “Transitioning from Breast Milk to Formula.” 8 Nov. 2009
<http://www.gerber.com/Articles/Transitioning_from_breastmilk_to_formula.aspx>.
Greene, Alan M.D., and Cheryl Greene.“How Much Milk Should Baby Be Drinking?
" drgreene.com. 11 Jan. 2010
<http://www.drgreene.com/21_857.html>.
---. "Introducing Solids." drgreene.com. 1 Dec. 2009. <http://www.drgreene.com/21_804.html>.
---."When Can Babies Start Solids?"drgreene.com. 1 Dec. 2009.
<http://www.drgreene.org/body.cfm?id=21&action=detail&ref=864>
Hogg, Tracy and Melinda Blau. Secrets of the Baby Whisperer: How to Calm, Connect, and
Communicate with Your Baby. New York: Ballantine, 2001.
La Leche League International (LLLI). "How Can I Tell If My Baby Is Getting Enough Milk?
" (Milk) La Leche League International. 14 Jan 2010
<http://www.llli.org/FAQ/enough.html>.
---. "How Do I Position My Baby to Breastfeed?" (Position) La Leche League
International.
19 Nov. 2009 <http://www.llli.org/FAQ/positioning.html>.
---. "What are the LLLI guidelines for storing my pumped milk?" (Storing)
La Leche League International.17 Nov 2010 <http://www.llli.org/FAQ/milkstorage.html>.
Salvatore, Silvia M.D., and Yvan Vandenplas M.D. "Gastroesophageal Reflux and Cow Milk Allergy: Is
There a Link?" Pediatrics: Official Journal of the American Academy of
Pediatrics.
110 (2002): 972-984. 30 Oct 2009 <http://pediatrics.aappublications.org>.
Sears, William M.D., Martha Sears, R.N., Robert Sears, M.D. and James Sears, M.D.
The Baby Book: Everything You Need to Know About Your Baby - From Birth
to Age Two. New York: Little, 2003.
Sears, William M.D., Martha Sears, R.N., James Sears, M.D., and Robert Sears, M.D.
"31 Ways to Get
Your Baby to Go to Sleep and Stay Asleep Easier." AskDrSears.com.
26 Jan 2010
<http://www.askdrsears.com/html/7/T070300.asp>.
Vickers, Melissa. “Finish the First Breast First.” LEAVEN September-October (1995): 69-71.
18 Nov. 2009. <http://www.llli.org/llleaderweb/LV/LVSepOct95p69a.html>.
Weissbluth, Marc M.D. Healthy Sleep Habits, Happy Child: A Step-By-Step Program for a
Good Night’s Sleep. New York: Ballantine, 2003.
 All Articles
All Articles All Videos
All Videos
 Hot Topics
Hot Topics Breastfeeding &
Breastfeeding &  Home
Home Videos
Videos Blog
Blog Bottle Feeding
Bottle Feeding Bottles
Bottles Formula
Formula Formula Transition
Formula Transition Nipples
Nipples Breastfeeding
Breastfeeding  To or Not To
To or Not To About
About Accessories
Accessories Pumping
Pumping Tips
Tips Comfort Chair
Comfort Chair Feeding Tricks
Feeding Tricks How Much?
How Much? Medical:
Medical: Storing
Storing Cereal
Cereal Water
Water Weaning
Weaning Bottle
Bottle Breast
Breast Nighttime
Nighttime Whole Milk
Whole Milk My Favorite
My Favorite  Resources
Resources Food
Food Home
Home Videos
Videos Blog
Blog Baby Cereal
Baby Cereal Baby Food
Baby Food Baby Food,
Baby Food, How Much to
How Much to Introducing
Introducing Medical:
Medical: Picky Eater
Picky Eater Top 10
Top 10 Water
Water Whole Milk
Whole Milk Organic
Organic Gift of Health
Gift of Health Grocery List
Grocery List Halloween
Halloween Healthy Snacks
Healthy Snacks Meal Ideas
Meal Ideas Dinner
Dinner Resources
Resources My Favorite
My Favorite Resources
Resources Household Items
Household Items Making Memories
Making Memories Home
Home Videos
Videos Blog
Blog Holidays
Holidays Easter Egg
Easter Egg Spring
Spring Summer
Summer Journal
Journal Memory of the Day
Memory of the Day Pictures
Pictures Holiday
Holiday Meal Time
Meal Time Monthly
Monthly Stories
Stories Medical
Medical Home
Home Blog
Blog Colic?
Colic? Reflux
Reflux About
About Coping
Coping Medication
Medication Autism
Autism How to Talk
How to Talk Sick
Sick Cold
Cold Ear Infection
Ear Infection Fever
Fever Middle of
Middle of  Vomiting
Vomiting My Favorite
My Favorite Resources
Resources Parenting
Parenting Home
Home Videos
Videos Blog
Blog Attachment
Attachment Baby Wearing
Baby Wearing About
About Products
Products Cry
Cry Colic?
Colic? Meanings
Meanings Get Easier?
Get Easier? Gift of Health
Gift of Health Nighttime
Nighttime Schedule
Schedule Schedule or Demand
Schedule or Demand Document
Document Template
Template Soothing Techniques
Soothing Techniques Toddlers, Loveable Puppies
Toddlers, Loveable Puppies Obstinate Ones
Obstinate Ones Autism
Autism How to Talk
How to Talk Reading Program
Reading Program Sexual
Sexual Stress Free
Stress Free My Favorite
My Favorite Resources
Resources Secrets
Secrets Play Time
Play Time Home
Home Videos
Videos Blog
Blog Costume
Costume  Crafts Ideas
Crafts Ideas Exercise
Exercise Triathlon
Triathlon Infant Play
Infant Play Toddler Play
Toddler Play Preschool Play
Preschool Play Preschool
Preschool  Home
Home Videos
Videos Colors
Colors Reading
Reading My Favorite
My Favorite Resources
Resources Pregnancy &
Pregnancy &  Home
Home Videos
Videos Blog
Blog Pregnancy
Pregnancy Baby Names
Baby Names For Mommy
For Mommy Prepare for
Prepare for  Baby
Baby Delivery
Delivery Take to
Take to Birth
Birth My Favorite
My Favorite Resources
Resources Secrets
Secrets Routine Care
Routine Care Home
Home Blog
Blog Baby Wearing
Baby Wearing About
About Products
Products Car Seat
Car Seat Child Care
Child Care Cry
Cry Colic?
Colic? Help Reduce
Help Reduce Meanings
Meanings Potty Training
Potty Training Reflux
Reflux About
About Coping
Coping Medication
Medication Soothing Techniques
Soothing Techniques Stroller
Stroller Sunblock
Sunblock Autism
Autism How to Talk
How to Talk Sexual
Sexual Stress Free
Stress Free My Favorite
My Favorite Resources
Resources Secrets
Secrets Sleep
Sleep Home
Home Videos
Videos Blog
Blog About
About Amount
Amount Comfort Chair
Comfort Chair Healthy Sleep
Healthy Sleep Nighttime
Nighttime Nightwaking
Nightwaking Behavior
Behavior Medical & Physical
Medical & Physical Parenting
Parenting Routine
Routine Sleep Tips
Sleep Tips Toddler/
Toddler/  You
You Stress Free
Stress Free My Favorite
My Favorite Resources
Resources Travel & Daily
Travel & Daily  Home
Home Blog
Blog Pool Time
Pool Time Holidays
Holidays Easter Egg
Easter Egg Spring
Spring Summer
Summer Vacation
Vacation Busch Gardens
Busch Gardens Busch Gardens Blog
Busch Gardens Blog My Favorite
My Favorite Resources
Resources My Family
My Family Home
Home Videos
Videos Blog
Blog About Me
About Me Journal
Journal Diary of a Mom
Diary of a Mom Diary of a Dad
Diary of a Dad Diary of a 3 Year Old
Diary of a 3 Year Old Diary of an Infant
Diary of an Infant I Love
I Love Let It Snow
Let It Snow Memory of the Day
Memory of the Day New Year's Resolutions
New Year's Resolutions Toddlers, Loveable Puppies
Toddlers, Loveable Puppies Washington Monument
Washington Monument You're a Mom
You're a Mom Meet My Family
Meet My Family Pictures
Pictures Holiday
Holiday Meal Time
Meal Time Monthly
Monthly Stories
Stories Vacation
Vacation Busch Gardens Blog
Busch Gardens Blog My Favorite Things
My Favorite Things Archives
Archives January
January 01/27/2012
01/27/2012 February
February 02/24/2012
02/24/2012 March
March 03/02/2012
03/02/2012 April
April 04/06/2012
04/06/2012 04/27/2012
04/27/2012 May - September
May - September 09/14/2012
09/14/2012 January
January 01/14/2011
01/14/2011 01/21/2011
01/21/2011 01/28/2011
01/28/2011 February
February 02/04/2011
02/04/2011 02/18/2011
02/18/2011 March
March 03/04/2011
03/04/2011 03/25/2011
03/25/2011 April
April 04/21/2011
04/21/2011 May
May 05/06/2011
05/06/2011 05/27/2011
05/27/2011 June
June 06/03/2011
06/03/2011 06/17/2011
06/17/2011 July
July 07/01/2011
07/01/2011 August
August 08/05/2011
08/05/2011 08/25/2011
08/25/2011 September
September 09/09/2011
09/09/2011 09/30/2011
09/30/2011 October
October 10/31/2011
10/31/2011 November
November 11/04/2011
11/04/2011 11/11/2011
11/11/2011 11/18/2011
11/18/2011 December
December 12/02/2011
12/02/2011 12/31/2011
12/31/2011 January
January 01/01/10
01/01/10 01/08/10
01/08/10 01/15/10
01/15/10 01/22/10
01/22/10 01/29/10
01/29/10 February
February 02/05/10
02/05/10 02/12/10
02/12/10 02/19/10
02/19/10 02/26/10
02/26/10 March
March 03/05/10
03/05/10 03/12/10
03/12/10 03/19/10
03/19/10 03/26/10
03/26/10 April
April 04/02/2010
04/02/2010 04/09/2010
04/09/2010 04/16/2010
04/16/2010 04/30/2010
04/30/2010 May
May 05/07/2010
05/07/2010 05/14/2010
05/14/2010 05/21/2010
05/21/2010 05/28/2010
05/28/2010 June
June 06/04/2010
06/04/2010 06/11/2010
06/11/2010 06/18/2010
06/18/2010 06/25/2010
06/25/2010 July
July 07/02/2010
07/02/2010 07/09/2010-
07/09/2010- 07/30/2010
07/30/2010 August
August 08/06/2010
08/06/2010 08/13/2010
08/13/2010 08/20/2010
08/20/2010 08/27/2010
08/27/2010 September
September 09/03/2010-
09/03/2010- 09/17/2010
09/17/2010 October
October 09/24/2010-
09/24/2010- 10/08/2010
10/08/2010 10/15/2010-
10/15/2010- November
November 11/05/2010
11/05/2010 11/12/2010
11/12/2010 11/19/2010
11/19/2010 December
December 12/17/2010
12/17/2010 October
October 10/30/09
10/30/09 November
November 11/13/09
11/13/09 11/20/09
11/20/09 11/27/09
11/27/09 December
December 12/04/09
12/04/09 12/11/09
12/11/09 12/18/09
12/18/09 12/25/09
12/25/09